 |
 |
| Korean J Ophthalmol > Volume 29(1); 2015 > Article |
Abstract
Purpose
Maltol (3-hydroxy-2-methyl-4-pyrone), formed by the thermal degradation of starch, is found in coffee, caramelized foods, and Korean ginseng root. This study investigated whether maltol could rescue neuroretinal cells from oxidative injury in vitro.
Methods
R28 cells, which are rat embryonic precursor neuroretinal cells, were exposed to hydrogen peroxide (H2O2, 0.0 to 1.5 mM) as an oxidative stress with or without maltol (0.0 to 1.0 mM). Cell viability was monitored with the lactate dehydrogenase assay and apoptosis was examined by the terminal deoxynucleotide transferase-mediated terminal uridine deoxynucleotidyl transferase nick end-labeling (TUNEL) method. To investigate the neuroprotective mechanism of maltol, the expression and phosphorylation of nuclear factor-kappa B (NF-κB), extracellular signal-regulated kinase (ERK), c-Jun N-terminal kinase (JNK), and p38 were evaluated by Western immunoblot analysis.
Results
R28 cells exposed to H2O2 were found to have decreased viability in a dose- and time-dependent manner. However, H2O2-induced cytotoxicity was decreased with the addition of maltol. When R28 cells were exposed to 1.0 mM H2O2 for 24 hours, the cytotoxicity was 60.69 ± 5.71%. However, the cytotoxicity was reduced in the presence of 1.0 mM maltol. This H2O2-induced cytotoxicity caused apoptosis of R28 cells, characterized by DNA fragmentation. Apoptosis of oxidatively-stressed R28 cells with 1.0 mM H2O2 was decreased with 1.0 mM maltol, as determined by the TUNEL method. Western blot analysis showed that treatment with maltol reduced phosphorylation of NF-κB, ERK, and JNK, but not p38. The neuroprotective effects of maltol seemed to be related to attenuated expression of NF-κB, ERK, and JNK.
Conclusions
Maltol not only increased cell viability but also attenuated DNA fragmentation. The results obtained here show that maltol has neuroprotective effects against hypoxia-induced neuroretinal cell damage in R28 cells, and its effects may act through the NF-κB and mitogen-activated protein kinase signaling pathways.
Glaucoma is a common eye condition that affects millions of individuals worldwide, making it the second-leading cause of blindness [1]. It is a generic term for a group of heterogeneous ocular neuropathies that eventually lead to gradual axonal degeneration in the optic nerve and progressive loss of retinal ganglion cells (RGCs). RGC death and optic nerve degeneration are complex processes with underlying molecular mechanisms that are only partially understood.
The most common treatment of glaucoma is the use of medications that lower intraocular pressure because increased intraocular pressure is the single most significant risk factor for the development and progression of glaucoma. However, treatments commonly used for glaucoma have little longterm value and only prolong the period over which degeneration occurs. Therefore, a neuroprotective medicine that can delay or prevent RGC loss is needed. Neuroprotective therapies work at the connection between damaging the optic nerve and loss of RGCs. Although recent studies of glaucoma have aimed to develop new treatment strategies to rescue the damaged RGCs with neuroprotective agents, currently there is no drug that shows significant neuroprotective effects.
Maltol (2-methyl-3-hydroxy-1,4-pyrone) is a naturally occurring substance that is widely used as a flavoring agent. It is formed through thermal degradation of starch or sucrose pyrolysis, and is found in baked products as well as Korean ginseng root, coffee, chicory, soybeans, bread crusts, and caramelized foods. Maltol is not only commonly used in breads, cakes, malt beverages, and chocolate milk as a flavor enhancer [2], but is also used in medications such as vanadyl maltolate for the treatment of diabetes, and ferric trimaltol for the treatment of iron deficiency anemia [3,4]. In previous studies, it has been reported that maltol has a neuroprotective effect through its antioxidant properties [5,6], and anti-apoptotic effects [7]. Although previous studies have shown that maltol attenuates neurotoxicity and prevents oxidative damage, there has been no comprehensive study of the protective effects of maltol on neurosensory retinal cells.
R28 cells are rat embryonic precursor neuroretinal cells originating from a postnatal day 6 rat retinal culture immortalized with the 12S E1A (NP-040507) gene of the adenovirus in a replication-incompetent viral vector [8]. R28 cells express genes characteristic of neurons [9], and have functional neuronal properties [10]. This study involved generating free radicals from hydrogen peroxide (H2O2) to oxidatively stress R28 cells, and investigated the protective effects of maltol and its underlying mechanisms.
R28 cells were purchased from KeraFAST (Boston, MA, USA). Cells were cultured in Dulbecco's modified Eagle's medium (Gibco, Carlsbad, CA, USA) supplemented with 10% fetal bovine serum (Gibco) and 100 µg/mL streptomycin (Gibco). Cells were passaged every 2 to 3 days and incubated at 37℃ in 5% CO2 to reach 80% confluence, and then they were transferred to a serum-free environment for 24 hours to reach a sessile, nonproliferative state.
Oxidative stress was caused by the addition of H2O2 (Sigma-Aldrich, St. Louis, MO, USA) to the culture media. R28 cells were exposed to several concentrations of H2O2 (0.0, 0.2, 0.4, 0.6, 0.8, 1.0, and 1.5 mM) for 48 hours. After 24 hours of exposure to 1.0 mM H2O2, 60% cell cytotoxicity was reached so a 24 hour exposure to 1.0 mM H2O2 was selected for oxidative stress conditions. Oxidatively-stressed R28 cells were then incubated with 0.0, 0.1, 0.5, 1.0, and 1.5 mM maltol (Sigma-Aldrich) for 24 hours.
Cell cytotoxicity was quantified by the measurement of lactate dehydrogenase (LDH) released into the culture media from damaged cells according to the manufacturer's instructions (CytoTox 96 non-radioactive cytotoxicity assay kit; Promega Corporation, Madison, WI, USA). The level of LDH release was normalized to the total LDH content following cell lysis in a medium. The absorbance was determined at 490 nm using a Multimode Microplate Reader (Berthold Technologies, Bad Wildbad, Germany). LDH release was expressed as a percentage of the maximum LDH released after cell lysis.
To analyze the occurrence of DNA fragmentation, the terminal deoxynucleotide transferase-mediated terminal uridine deoxynucleotidyl transferase nick end-labeling (TUNEL) assay (BD Biosciences Pharmingen, San Diego, CA, USA) was used. R28 cells were plated in 6-well tissue culture plates at a cell density of 2.0 × 105 cells per well. The cells were treated for 16 hours with the compounds. The cells were removed by trypsinization, washed twice with phosphate-buffered saline and fixed for 1 hour in 1% paraformaldehyde. The cells were washed twice with phosphate-buffered saline and perrmeabilized for 48 hours in 70% ethanol at -20℃. Transferred bromolated deoxyuridine triphosphate nucleotides (Br-dUTP) to the free 3'-OH of cleaved DNA by terminal deoxynucleotide transferase were detected by the anti-BrdU-fluorescein isothyocyanate (FITC) antibody under fluorescence microscopy. Subsequently the cells were labeled with FITC-dUTP and propidium iodide as described in the manufacturer's manual (BD Biosciences Pharmingen).
For extraction of whole cellular proteins, cells were washed twice with ice-cold phosphate buffered saline and then lysed with cell lysis buffer (50 mM Tris-HCl pH 7.4, 1% NP-40, 0.25% Na-deoxycholate, 150 mM NaCl, 1 mM EDTA, 10 mM Na3VO4, 50 mM NaF, 1 mM PMSF, 1 µg/mL aprotinin, 1 µg/mL leupeptin, 1 µg/mL pepstatin) on ice for 30 minutes. Lysates were sonicated, and the cell homogenates were centrifuged at 15,000 g for 10 minutes (4℃). After centrifugation, supernatants were electrophoresed in 10% acrylamide gels and transferred onto nitrocellulose membranes. The proteins were probed overnight with antibodies against JNK, ERK p44/42, p38, NF-κB p65, phospho-JNK, phospho-ERK p44/42, phospho-p38, phospho-NF-κB (Cell Signaling Technology, Danvers, MA, USA) and β-actin (Santa Cruz Biotechnology, Santa Cruz, CA, USA). The immunoreactive bands were detected with horseradish peroxidase-conjugated secondary antibodies and visualized by enhanced chemiluminescence.
Data are expressed as the mean ± SD of at least three different experiments performed from separate cell preparations, and at least triplicate determinations were performed for each experiment. Statistical tests to determine differences between groups were performed with one-way analysis of variance, followed by the post hoc Tukey test using SPSS ver. 17.0 (SPSS Inc., Chicago, IL, USA). A p-value of less than 0.05 was considered statistically significant.
R28 cells were exposed to 0.0, 0.2, 0.4, 0.6, 0.8, 1.0, and 1.5 mM H2O2 for 24 hours and exposed to 1.0 mM H2O2 for 1, 3, 6, 16, 24 and 48 hours. Cytotoxicity was quantified by measurement of released LDH to culture media from injured cells. As shown in Fig. 1, H2O2 increased LDH release in a dose- and time-dependent manner. When R28 cells were exposed to 1.0 mM H2O2 for 24 hours, the cytotoxicity was 60.69 ± 5.71%. The 24 hours of exposure to 1.0 mM H2O2 was selected as the oxidative stress conditions for further experiments.
R28 cells were co-cultured with 1.0 mM H2O2 and different concentrations of maltol ranging from 0.1 to 1.5 mM for 24 hours. Co-culture with maltol attenuated H2O2-induced cytotoxicity in a dose-dependent manner (Fig. 2). When compared to 1.0 mM H2O2 treated cells, the protective effect of 0.1 mM maltol was not statistically different, but 0.5, 1.0 and 1.5 mM maltol significantly decreased LDH leakage from injured cells. LDH leakage markedly increased with the addition of 1.0 mM H2O2 (59.25 ± 2.81%) when compared to a control (10.48 ± 1.80%, p < 0.05). However, 1.0 mM maltol treatment significantly attenuated these cytotoxic effects (19.86 ± 1.11%). To investigate the underlying mechanism of the neuroprotective effects of maltol, the co-culture condition of 1.0 mM H2O2 and 1.0 mM maltol was selected for following experiments.
In Fig. 3, the TUNEL assay for broken DNA from apoptotic cells revealed a FITC (green fluorescence)-positive signal. Propidium iodide counter-staining demonstrated living cells (red fluorescence). After co-culture with 1.0 mM maltol, R28 cells became more resistant to H2O2-induced oxidative stress injury. The ratio of TUNEL positive apoptotic cells to the total number of cells increased with the addition of 1.0 mM H2O2 (16.33 ± 2.31%) when compared to a control (1.72 ± 0.31 %, p < 0.05). However, the ratio decreased with co-culture of 1.0 mM maltol (2.64 ± 0.52 %). Maltol treatment markedly reduced the loss of R28 cells possibly through a decrease in apoptosis.
To investigate the neuroprotective mechanism of maltol, the expression of nuclear factor-kappa B (NF-κB), extracellular signal-regulated kinase (ERK), c-Jun N-terminal kinase (JNK) and p38 were evaluated by Western immunoblot analysis. Fig. 4A shows the protein expression of phospho-NF-κB, phospho-JNK, phospho-ERK, phospho-p38, and β-actin after 48 hours with or without 1.0 mM maltol in R28 cells exposed to 1.0 mM H2O2. The expression of phospho-NF-κB, phospho-JNK, and phospho-ERK decreased with co-culture of 1.0 mM maltol, especially after 2 hours of H2O2 exposure. However, the expression of phospho-p38 showed no difference in the presence or absence of maltol. To quantify protein expression within 2 hours after exposure to 1.0 mM H2O2, the band intensities were measured with the ImageJ program (ImageJ Software; National Institute of Health, Bethesda, MD, USA). Fig. 4B shows that the expression levels of phospho-NF-κB, phospho-JNK, and phospho-ERK were 2.16-, 7.7-, and 4.3-times higher than those of a control, and these expression levels were significantly decreased with the addition of 1.0 mM maltol to 1.18-, 2.3-, and 1.8-times higher than those of the control, respectively. However, there was not significant change in phospho-p38 expression in oxidatively-stressed R28 cells at 1.7-times higher levels than control without maltol and 1.8-times with maltol.
Maltol has been reported to have various biologic functions such as being a natural scavenger of reactive oxygen species [6], and as a mediator of enhanced mitochondrial function, reduced intracellular calcium, and reduced expression of NF-κB [7]. However, its effects and underlying mechanisms of action in neurosensory retinal cells have not been previously reported. In the present study, maltol not only increased cell viability but also attenuated DNA fragmentation. The results here show that maltol has neuroprotective effects against hypoxia-induced neurosensory retinal cell damage in R28 cells and its effects may act through the NFκB and mitogen-activated protein kinase (MAPK) signaling pathways.
NF-κB is an important transcription factor that regulates the stimulus-dependent induction of genes critical to the survival and death of neurons [11,12]. Various stimuli such as stress and cytokines can activate NF-κB, and then the activated form of phosphorylated NF-κB enters the nucleus and initiates the expression of genes to determine cell survival or death [13,14]. Wu et al. [15] reported that in light-induced photoreceptor degeneration, NF-κB was activated and exhibited neuroprotective and anti-apoptotic functions. However, Grilli et al. [16] reported that in glutamate-induced neurotoxicity, blockade of NF-κB activation was found to be protective. Therefore, NF-κB activation may induce both anti- and pro-apoptotic effects on different cells or under different pathological conditions. Previously, the activated NF-κB has been reported to participate in glutamate-induced neurotoxicity, N-methyl-D-aspartate (NMDA)-induced retinal neuronal cell death, retinal ischemia, and reperfusion injury [16,17,18,19]. In this study, phosphorylated NF-κB was increased in oxidatively-stressed R28 cells by H2O2, but was decreased when co-cultured with maltol. This finding is consistent with the results from previous studies. Yang et al. [7] reported that maltol could reduce NF-κB activated by H2O2 and prevent H2O2-induced apoptosis in human neuroblastoma cells (SH-SY5Y). This result shows that the neuroprotective effect of maltol is mediated by reduction of activated NF-κB.
The MAPK family consists of three main protein kinase families: the ERKs, JNKs, and p38 family of kinases. MAPK pathways have crucial roles in the regulation of cellular activities including proliferation, differentiation, survival, death, and cellular responses to external stresses. Activation of ERKs typically contributes to cell differentiation, proliferation, and survival, whereas JNK and p38 are, in contrast, activated by pro-inflammatory cytokines and environmental stress and have been suggested to promote apoptosis.
The present study showed that there were significant changes of phosphorylated ERK in oxidatively-stressed R28 cells with or without maltol treatment. Previous studies reported that ERK activation is a major factor related to cell survival [20,21,22]. However, in the present study, activated phosphorylated ERK decreased with maltol treatment in oxidatively-stressed R28 cells. The present findings are in apparent contrast to the above-mentioned studies. However, Luo et al. [23] demonstrated that inhibition of the ERK pathway promotes RGC survival and axon regeneration, probably via preventing excitotoxic amino acid release or blockade of nonapoptotic processes after optic nerve injury. Additionally, Cagnol et al. [24] reported that prolonged activation of the ERK pathway induces activation of pro-apoptotic caspase-8, and Stanciu et al. [25] reported that ERK activation is involved in glutamate and NMDA receptor-mediated neurotoxicity. The current study does not provide enough evidence to clarify the controversial role of the ERK pathway, because ERK activation could be interpreted as having both anti- and pro-apoptotic effects. Maltol may have a neuroprotective effect through down-regulation of phosphorylated ERK as a pro-apoptotic signal, or maltol may sufficiently reduce the oxidative stress on RGCs such that ERK cannot be activated as an anti-apoptotic signal. Although the role of phosphorylated ERK has not been clarified, the neuroprotective mechanism of maltol has been found to be associated with the ERK pathway in oxidatively-stressed R28 cells.
In this study, phosphorylated JNK was increased in oxidatively-stressed R28 cells and decreased with maltol addition. Previous studies demonstrated that oxidative stress-induced apoptosis was commonly mediated by the activation of JNK pathways [26]. The present study also showed that H2O2 induced activation of JNK and was suppressed by maltol addition. These results suggest that maltol may suppress the pro-apoptotic effect mediated by downregulation of phosphorylated JNK. On the other hand, there was no significant change in phospho-p38 in oxidatively-stressed R28 cells in the presence or absence of maltol. In the present study, phospho-p38 was found to increase less than phospho-ERK and JNK, at 1.7-, 7.7-, and 4.3-times higher than a control, respectively. Although p38 and JNK are often coactivated, specific activation of p38 and JNK has been observed, implying that there is specific activation of p38 or JNK. For example, Ogura and Kitamura [27] demonstrated that treatment of macrophages with menadione rapidly induced phosphorylation of ERK and p38 MAP kinase, but not JNK. The present study also showed that in oxidatively-stressed R28 cells, the p38 pathway was less influenced than other MAPK pathways.
R28 cells have both glial and neuronal characteristics, and have been widely used to elucidate the molecular mechanism of neuronal apoptosis in the retina [28]. However, the RGCs comprise only a very small fraction of retinal cells (one per ten thousand) and R28 cells do not behave like primary RGCs in every aspect. This is a potential limitation of the present study. However, isolating and culturing primary RGCs are technically difficult and widely used RGC-5 cells, once thought to be a rat RGC line [29], are now reported to express photoreceptor markers that are also expressed in the unrelated SV40-transformed mouse photoreceptor cell line 661W [30,31]. Use of this crosscontaminated and uncharacterized cell line could result in erroneous scientific conclusions. Therefore, the goal of this study was to use the R28 cell line to determine the neuroprotective effect of maltol with the expectation that the in vitro data set obtained from R28 cells can be verified in primary RGCs in a future study. Further, an in vitro cell line that is easy to handle and better represents RGC characteristics should be developed.
In this study, maltol was found to have a neuroprotective effect against H2O2-induced cytotoxicity in R28 cells. However, maltol has been reported to have weak mutagenic activity and toxic effects mediated through apoptosis [32]. However, at the recommended concentration, maltol does not have any toxic effect. The UN Joint FAO/WHO Export Committee on Food Additives concluded that up to 1 mg/kg per day was an acceptable level of consumption for human beings [2]. For dogs and rats, maltol showed no adverse toxic effect at doses up to and including 200 mg/kg/day for 2 years [33]. Also, Kim et al. [6] reported that maltol had a neuroprotective effect against oxidative stress in the brains of mice challenged with kainic acid at a dose of 100 mg/kg for 5 consecutive days. Previous in vitro studies showed that concentrations ranging from 50 to 1,000 µM did not significantly affect cell viability, but a concentration of 10 mM decreased cell viability to 75% [34]. Based on these findings, the present studies were conducted at concentrations of maltol ranging from 0.1 to 1.5 mM.
In conclusion, the present study demonstrates that maltol inhibits apoptosis of R28 cells induced by H2O2. The mechanisms underlying this protection are not fully understood but are associated with NF-κB and MAPK-related pathways. This study provides evidence that maltol could be an innovative neuroprotective therapeutic agent for the reduction of neurosensory retinal cell injury related to hypoxia.
Notes
This work was presented as poster at the Annual Meeting of the Korean Ophthalmological Society, Busan, Korea, April 11-13, 2014.
REFERENCES
1. Quigley HA, Broman AT. The number of people with glaucoma worldwide in 2010 and 2020. Br J Ophthalmol 2006;90:262-267.



2. Joint FAO/WHO Expert Committee on Food Additives. Evaluation of certain veterinary drug residues in food: sixty-sixth report of the Joint FAO/WHO Expert Committee on Food Additives. World Health Organ Tech Rep Ser 2006;(939):1-80.
3. Harvey RS, Reffitt DM, Doig LA, et al. Ferric trimaltol corrects iron deficiency anaemia in patients intolerant of iron. Aliment Pharmacol Ther 1998;12:845-848.


4. Thompson KH, Liboiron BD, Sun Y, et al. Preparation and characterization of vanadyl complexes with bidentate maltol-type ligands: in vivo comparisons of anti-diabetic therapeutic potential. J Biol Inorg Chem 2003;8:66-74.


5. Hong YL, Pan HZ, Scott MD, Meshnick SR. Activated oxygen generation by a primaquine metabolite: inhibition by antioxidants derived from Chinese herbal remedies. Free Radic Biol Med 1992;12:213-218.


6. Kim YB, Oh SH, Sok DE, Kim MR. Neuroprotective effect of maltol against oxidative stress in brain of mice challenged with kainic acid. Nutr Neurosci 2004;7:33-39.


7. Yang Y, Wang J, Xu C, et al. Maltol inhibits apoptosis of human neuroblastoma cells induced by hydrogen peroxide. J Biochem Mol Biol 2006;39:145-149.


8. Seigel GM. Establishment of an E1A-immortalized retinal cell culture. In Vitro Cell Dev Biol Anim 1996;32:66-68.


9. Seigel GM, Sun W, Wang J, et al. Neuronal gene expression and function in the growth-stimulated R28 retinal precursor cell line. Curr Eye Res 2004;28:257-269.


10. Sun W, Seigel GM, Salvi RJ. Retinal precursor cells express functional ionotropic glutamate and GABA receptors. Neuroreport 2002;13:2421-2424.


11. Ghosh S, May MJ, Kopp EB. NF-kappa B and Rel proteins: evolutionarily conserved mediators of immune responses. Annu Rev Immunol 1998;16:225-260.


12. Van Antwerp DJ, Verma IM. Signal-induced degradation of I(kappa)B(alpha): association with NF-kappaB and the PEST sequence in I(kappa)B(alpha) are not required. Mol Cell Biol 1996;16:6037-6045.



14. Gilmore TD. Introduction to NF-kappaB: players, pathways, perspectives. Oncogene 2006;25:6680-6684.


15. Wu T, Chiang SK, Chau FY, Tso MO. Light-induced photoreceptor degeneration may involve the NF kappa B/caspase-1 pathway in vivo. Brain Res 2003;967:19-26.


16. Grilli M, Pizzi M, Memo M, Spano P. Neuroprotection by aspirin and sodium salicylate through blockade of NF-kappaB activation. Science 1996;274:1383-1385.


17. Nakai M, Qin ZH, Chen JF, et al. Kainic acid-induced apoptosis in rat striatum is associated with nuclear factor-kappaB activation. J Neurochem 2000;74:647-658.


18. Fan W, Cooper NG. Glutamate-induced NFkappaB activation in the retina. Invest Ophthalmol Vis Sci 2009;50:917-925.


19. Chen YG, Zhang C, Chiang SK, et al. Increased nuclear factor-kappa B p65 immunoreactivity following retinal ischemia and reperfusion injury in mice. J Neurosci Res 2003;72:125-131.


20. Gupta VK, You Y, Li JC, et al. Protective effects of 7,8-dihydroxyflavone on retinal ganglion and RGC-5 cells against excitotoxic and oxidative stress. J Mol Neurosci 2013;49:96-104.


21. Zhou Y, Pernet V, Hauswirth WW, Di Polo A. Activation of the extracellular signal-regulated kinase 1/2 pathway by AAV gene transfer protects retinal ganglion cells in glaucoma. Mol Ther 2005;12:402-412.


22. Pernet V, Hauswirth WW, Di Polo A. Extracellular signal-regulated kinase 1/2 mediates survival, but not axon regeneration, of adult injured central nervous system neurons in vivo. J Neurochem 2005;93:72-83.


23. Luo JM, Cen LP, Zhang XM, et al. PI3K/akt, JAK/STAT and MEK/ERK pathway inhibition protects retinal ganglion cells via different mechanisms after optic nerve injury. Eur J Neurosci 2007;26:828-842.


24. Cagnol S, Van Obberghen-Schilling E, Chambard JC. Prolonged activation of ERK1,2 induces FADD-independent caspase 8 activation and cell death. Apoptosis 2006;11:337-346.


25. Stanciu M, Wang Y, Kentor R, et al. Persistent activation of ERK contributes to glutamate-induced oxidative toxicity in a neuronal cell line and primary cortical neuron cultures. J Biol Chem 2000;275:12200-12206.


26. Basu K, Mukhopadhyay A, Ghosh I, Datta K. Nuclear morphology and c-Jun N-terminal kinase 1 expression differentiate serum-starved oxidative stress signalling from hydrogen peroxide-induced apoptosis in retinal neuronal cell line. Cell Biol Int 2012;36:1021-1027.


27. Ogura M, Kitamura M. Oxidant stress incites spreading of macrophages via extracellular signal-regulated kinases and p38 mitogen-activated protein kinase. J Immunol 1998;161:3569-3574.



29. Krishnamoorthy RR, Agarwal P, Prasanna G, et al. Characterization of a transformed rat retinal ganglion cell line. Brain Res Mol Brain Res 2001;86:1-12.


31. Krishnamoorthy RR, Clark AF, Daudt D, et al. A forensic path to RGC-5 cell line identification: lessons learned. Invest Ophthalmol Vis Sci 2013;54:5712-5719.


32. Hironishi M, Kordek R, Yanagihara R, Garruto RM. Maltol (3-hydroxy-2-methyl-4-pyrone) toxicity in neuroblastoma cell lines and primary murine fetal hippocampal neuronal cultures. Neurodegeneration 1996;5:325-329.


Fig. 1
Hydrogen peroxide (H2O2) induced cytotoxicity in R28 cells. (A) R28 cells were exposed to H2O2 ranging from 0.0 to 1.5 mM for 24 hours. (B) R28 cells were exposed to 1.0 mM H2O2 for up to 48 hours. Cell cytotoxicity was quantified by an lactate dehydrogenase assay. H2O2 increased lactate dehydrogenase release in a dose- and time-dependent manner. When R28 cells were exposed to 1.0 mM H2O2 for 24 hours, the cytotoxicity was 60.69 ± 5.71%. Data are expressed as the mean ± SD.

Fig. 2
The protective effect of maltol treatment (bright field microscopy). (A) Control. (B) R28 cells exposed to 1.0 mM hydrogen peroxide (H2O2). (C) R28 cells exposed to 1.0 mM maltol. (D) R28 cells co-cultured with 1.0 mM H2O2 and 1.0 mM maltol. (E) R28 cells were co-cultured with 1.0 mM H2O2 and different concentrations of maltol ranging from 0.1 to 1.5 mM for 24 hours. Cell cytotoxicity was quantified by an lactate dehydrogenase assay. Maltol decreased lactate dehydrogenase leakage from injured cells in a dose-dependent manner. Scale bar in panels (A) to (D) = 50 µm. Data are expressed as mean ± SD (the asterisks denote that data are significantly different from the untreated control; *1.0 mM H2O2-treated cells; **p < 0.05).
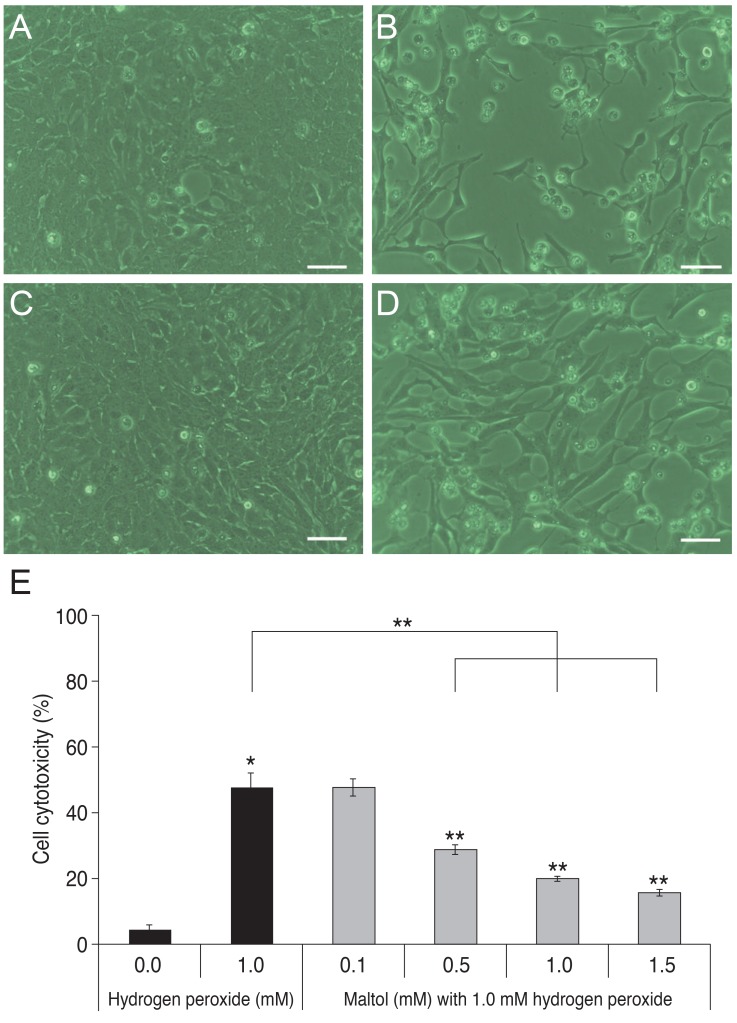
Fig. 3
Anti-apoptotic effects of maltol treatment. (A-C) Representative photographs of terminal deoxynucleotide transferase-mediated terminal uridine deoxynucleotidyl transferase nick end-labeling (TUNEL), in which green fluorescence indicates apoptotic cells and red fluorescence indicates living cells. (A) Control. (B) 1.0 mM hydrogen peroxide (H2O2). (C) 1.0 mM H2O2 with 1.0 mM maltol. (D) Quantification of TUNEL-positive cells; data collected from 10 fields for each group; experiments were repeated three times. Data are expressed as mean ± SD of the ratio of apoptotic cells to the total number of cells. After co-culture with 1.0 mM maltol, oxidatively-stressed R28 cells became more resistant to hydrogen peroxide injury (the asterisks denote that data are significantly different from control; *p < 0.05).

Fig. 4
Western blot analysis of nuclear factor-kappa B (NF-κB) and mitogen-activated protein kinase in R28 cells. (A) The expression of phospho NF-κB (pNF-κB), phospho c-Jun N-terminal kinase (pJNK), phospho extracellular signal-regulated kinase (pERK), phospho-p38 (pp38), and β-actin after 48 hours with or without 1.0 mM maltol in R28 cells exposed to 1.0 mM hydrogen peroxide (H2O2). (B) The band intensities, relative to a control in R28 cells exposed to 1.0 mM H2O2 within 2 hours. The black box indicates exposure to H2O2 without maltol treatment and the patterned box indicates exposure to H2O2 with maltol treatment. The expression of pNF-κB, pJNK, and pERK was reduced with 1.0 mM maltol treatment. However, there was no significant change of phospho-p38 in the presence or absence of maltol treatment. Data are expressed as mean ± SD (the asterisks denote that data are significantly different from 1.0 mM H2O2-treated cells, *p < 0.05).




 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print




