Uveal Melanoma with Massive Extraocular Extension through the Sclerocorneal Limbus
Article information
Dear Editor,
A 52-year-old male was referred to our institution because of an intraocular mass in his right eye. An elevated mass was found behind the iris. Ultrasonography revealed a solid mass and exudative retinal detachment in the lower retina. We recommended further evaluation and suspected ciliary body melanoma; however, the patient was lost to follow-up.
Four years later, the patient presented with a progressively protruding mass that had developed over the previous 3 months. A large dark-pigmented extraocular mass filled the entire right eyelid fissure (Fig. 1A). The mass seemed to be an anterior extraocular extension of the previously identified ciliary body melanoma via the superonasal corneoscleral limbus. Magnetic resonance imaging revealed a mass that occupied most of the vitreous cavity with invasion into the sclera. The lesion demonstrated marked hypointensity and hyperintensity on T2- and T1-weighted images, respectively. After gadolinium enhancement, the lesion demonstrated homogeneous intense enhancement that was strongly suggestive of melanoma (Fig. 1B). Positron emission tomography-computerized tomography revealed no distant metastasis.
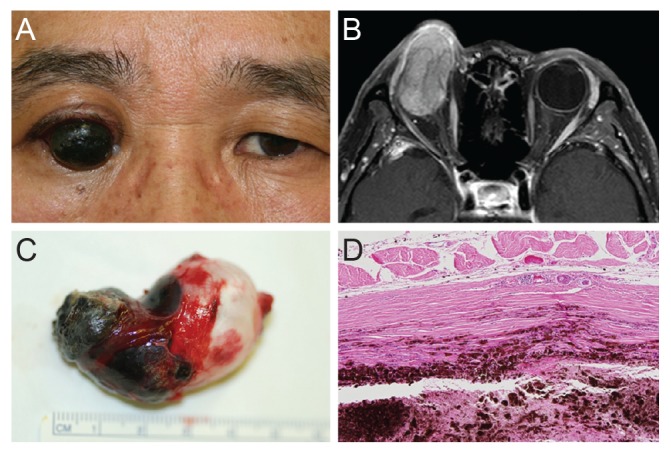
(A) The patient presented 4 years after the initial visit with a protruding dark-pigmented extraocular mass that filled the entire right eyelid fissure. (B) Gadolinium-enhanced T1-weighted magnetic resonance image showed an intraocular mass that occupied most of the vitreous cavity and had a massive anterior extraocular extension, but did not involve the optic nerve. (C) Enucleated eyeball with anterior extraocular extension of the uveal melanoma through the sclerocorneal limbus. The tumor measured 4.7 × 2.5 × 2.4 cm. (D) Melanin pigments dispersed throughout the scleral tissue, indicating scleral invasion, but the invasion did not reach the outermost layer of the sclera or the vessels (hematoxylin and eosin staining, ×100).
Enucleation was performed with additional resection of the tumor-surrounding conjunctiva, using the no-touch isolation technique. After removing the eyeball as well as the tumor, a 20-mm porous polyethylene implant (MEDPOR; Stryker Inc., Kalamazoo, MI, USA) was inserted into the anophthalmic cavity. Histopathological examination revealed a 47 × 25 × 24-mm-sized solid mass that involved the entire eyeball cavity (Fig. 1C). Tumor cells were compatible with spindle cell melanoma. The melanin pigment was dispersed throughout the scleral tissue, thereby indicating scleral invasion (Fig. 1D), but there was no tumor invasion into the optic nerve. No postoperative adjuvant treatment was performed. The patient demonstrated a good clinical course without local recurrence or distant metastasis for 36 months after the operation.
Melanomas that arise from the ocular and adnexal structures comprise 5% of all melanomas, and 85% of them originate from the uvea [1]. Extraocular extension of uveal melanoma is rare and difficult to manage. In a retrospective study performed on 610 patients with uveal melanoma, 50 patients (8.2%) had extrascleral extension and 16 patients (2.6%) had a large extended mass >4 mm. The 5-year survival rate was 22%, which is significantly lower than patients with smaller melanomas [2].
The tumor in this case was 47 × 25 × 24 mm in size, which, to the best of our knowledge, is the largest of this type of tumor that has been recorded. Shields et al. reported that the largest basal diameters of uveal melanomas identified in 8,033 eyes ranged between 1.0 to 33.0 mm [3]. Given the availability of advanced techniques for early detection as well as effective treatment, it is very rare to observe such a massive uveal melanoma with extraocular extension, in addition to the natural course of expansion.
Managing patients with uveal melanoma and extraocular extension remains controversial. Cases with macroscopic extrascleral extension are generally treated by enucleation or, in selected cases, orbital exenteration. However, Kersten et al. [4] reported that exenteration is palliative and prognosis is unaltered in patients who receive exenteration. Some reports suggest that adjunctive radiation treatment should be considered if the tumor is transected at the time of surgical removal [2]. Some reports on uveal melanomas with anterior extraocular extension have been managed using enucleation or exenteration. Kimura et al. [5] reported a 64-year-old female with anterior extraocular extension and mixed-cell melanoma through the sclera who underwent enucleation and adjuvant chemotherapy, but died of systemic metastasis at 6-months post-procedure.
In our case, the patient presented with some factors that were related to poor prognosis, such as the large ciliary body tumor, older age, male sex, and massive extraocular extension, but we only performed enucleation instead of aggressive orbital exenteration or adjuvant treatment for the following reasons: 1) the large size was due to anterior extraocular extension, but no tumor involvement was noted in the adjacent conjunctiva or eyelids; 2) preoperative magnetic resonance imaging provided no evidence of tumor invasion into the optic nerve or other orbital spaces; 3) positron emission tomography-computerized tomography revealed no distant metastasis; and 4) postoperative histopathology confirmed spindle-cell melanoma. To the best of our knowledge, this is the largest uveal melanoma reported to date with extraocular extension through the corneoscleral limbus. In cases without significant invasion into the adjacent ocular adnexal tissue or metastasis, we believe uveal melanoma with anterior extraocular extension can be managed by enucleation alone regardless of size.
Notes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.