The Short-term Efficacy of Subthreshold Micropulse Yellow (577-nm) Laser Photocoagulation for Diabetic Macular Edema
Article information
Abstract
Purpose
This pilot study aimed to evaluate the efficacy and safety of subthreshold micropulse yellow (577-nm) laser photocoagulation (SMYLP) in the treatment of diabetic macular edema (DME).
Methods
We reviewed 14 eyes of 12 patients with DME who underwent SMYLP with a 15% duty cycle at an energy level immediately below that of the test burn. The laser exposure time was 20 ms and the spot diameter was 100 µm. Laser pulses were administered in a confluent, repetitive manner with a 3 × 3 pattern mode.
Results
The mean follow-up time was 7.9 ± 1.6 months. The baseline-corrected visual acuity was 0.51 ± 0.42 logarithm of the minimum angle of resolution (logMAR), which was improved to 0.40 ± 0.35 logMAR (p = 0.025) at the final follow-up. The central macular thickness at baseline was 385.0 ± 111.0 µm; this value changed to 327.0 ± 87.7 µm (p = 0.055) at the final follow-up.
Conclusions
SMYLP showed short-term efficacy in the treatment of DME and did not result in retinal damage. However, prospective, comparative studies are needed to better evaluate the efficacy and safety of this treatment.
Laser photocoagulation in the macula has long been recognized as an effective treatment for diabetic macular edema (DME). The Early Treatment Diabetic Retinopathy Study (ETDRS) demonstrated a significant benefit of laser photocoagulation for the treatment of clinically significant macular edema, reducing the incidence of visual loss by approximately 50% at three-year follow-up [1,2]. The original ETDRS photocoagulation technique was adopted worldwide and was gradually modified over the years to become the present modified ETDRS focal/grid photocoagulation protocol, which, according to a survey of the DRCR.net (Diabetic Retinopathy Clinical Research Network), reflects the treatment approach currently used by most retinal specialists [2,3].
Despite the satisfactory results achieved, conventional laser photocoagulation causes visible laser scars that can continue to enlarge markedly during the long postoperative period [4]. This may lead to several complications over the long term, such as subretinal fibrosis, choroidal neovascularization, and field sensitivity deterioration, which can severely affect visual function [5,6,7,8,9,10,11]. Therefore, a less invasive treatment strategy has been advocated to reduce the application of laser energy and avoid tissue damage. Recent discernment of the modification of gene expression mediated by the healing response of the retinal pigment epithelium (RPE) to thermal injury suggests that the useful therapeutic cellular cascade is not activated by laser-killed RPE cells, but rather by the still-viable RPE cells surrounding the burned areas, which are reached by heat diffusion at sub-lethal thermal elevations [2,12,13].
Advances in laser technology have led to the development of selective photocoagulation for the RPE via the subthreshold micropulse laser photocoagulation method. This is designed to target the RPE, while having a minimal effect on the sensory retina and choroid. In 1997, Friberg and Karatza [14] first reported the clinical application of micropulse 810-nm diode laser therapy for DME. Several clinical studies have since demonstrated the efficacy of this method [2,3,15,16,17,18].
A new semiconductor laser device now provides cost-effective, reliable, solid-state 577-nm yellow laser light. Theoretically, the 577-nm yellow laser light provides peak absorption of oxyhemoglobin, excellent lesion visibility, low intraocular light scattering and pain, and negligible xanthophyll absorption [19,20]. Additionally, the 577-nm yellow laser wavelength has the advantage of being better absorbed by melanin than the 810-nm laser wavelength, a characteristic that is theoretically suited to the micropulse technique aimed at RPE cells. The 577-nm wavelength is outside the absorption spectrum of retinal xanthophylls, which potentially facilitates treatment of areas close to the fovea.
Although this laser system was recently commercialized, no clinical studies of the system have been reported to date. This 577-nm yellow laser system (Supra 577Y Laser System; Quantel Medical, Clermont-Ferrand, France) has been used for retinal treatment in our clinic since June 2010. The purpose of this pilot study was to evaluate the effects of subthreshold micropulse yellow laser photocoagulation (SMYLP) on eyes with DME using this laser system.
Materials and Methods
The medical records of all patients who underwent SMYLP for DME at the Retina Center of Nune Eye Hospital between June and December 2010 were reviewed. All patients underwent a chart review in addition to comprehensive ocular examinations, including anterior segment examination, dilated biomicroscopic examination of the macula, and a retinal evaluation with the Goldmann three-mirror contact lens. Visual acuity (VA) was determined using a decimal VA chart, and the decimal VA was converted to the logarithm of the minimum angle of resolution (logMAR) units for statistical analysis. Color fundus photography, fundus autofluorescence, and fluorescein angiography were performed to detect any laser damage and changes in macular edema before and after SMYLP.
To be eligible for the study, patients had to meet the following criteria: be at least 18 years of age and have a history of diabetes mellitus; have a recent history of visual deterioration; have a cystic macular lesion detected by optical coherence tomography (OCT) and/or a central macular thickness (CMT) >260 micron. OCT had to be performed within one week before SMYLP as well as during every follow-up visit.
Patients were excluded if they had a history of panretinal photocoagulation or conventional laser photocoagulation, if they had received antivascular endothelial growth factor treatments in the past four months, or if they had undergone major ocular surgery (including pars plana vitrectomy and cataract surgery) within six months before and after SMYLP. However, HbA1c, duration of diabetes mellitus, and severity of diabetic retinopathy were not considered criteria for exclusion. Informed consent was obtained from each patient. This study adhered to the ethical standards in the declaration of Helsinki, and was approved by the Institutional Review Board of Nune Eye Hospital, Seoul, Korea.
Of the 47 eyes of the 36 patients whose records were reviewed, 14 eyes of 12 patients were included in the study. Thirty-three eyes from 24 patients were excluded due to previous laser treatment or anti-vascular endothelial growth factor (VEGF) treatment (n = 15 eyes), anti-VEGF treatment and/or cataract surgery after SMYLP (n = 5 eyes), or because the patients were lost to follow-up (n = 13 eyes). In the five eyes (four patients) that received anti-VEGF treatment after SMYLP, three eyes (two patients) underwent cataract surgery with bevacizumab injection to prevent aggravation of macular edema and the other two patients (two eyes) refused repetitive SMYLP and requested anti-VEGF treatment for faster improvement of vision. All patients underwent spectral domain (SD) OCT (Spectralis; Heidelberg Engineering, Heidelberg, Germany).
All treatments were provided with the 577-nm yellow laser system (Supra 577Y Laser System). Laser application was performed with an Area-Centralis lens (Volk Optical, Mentor, OH, USA), and the micropulse laser power used in SMYLP was derived for each eye from a test burn. The test burn was performed with a 577-nm yellow laser in the continuous-wave (CW) mode using a 100-µm spot diameter and a 20 ms duration outside the vascular arcade with the power titrated from 100 mW upward until a burn became barely visible. The subthreshold treatment was then performed with the same spot size by switching the laser from the CW to the micropulse mode at the onset of the 15% duty cycle (0.18 ms "on" time and 1 ms "off" time) for 20 ms at an energy level immediately below the threshold (100 to 180 mW) used for a test burn. Laser shots were delivered together in a 3 × 3 pattern mode (1.5 widths) over the entire area of macular edema including the foveal center (Fig. 1). The SMYLP was repeated after 1 to 2 months if DME persisted on SD-OCT images.
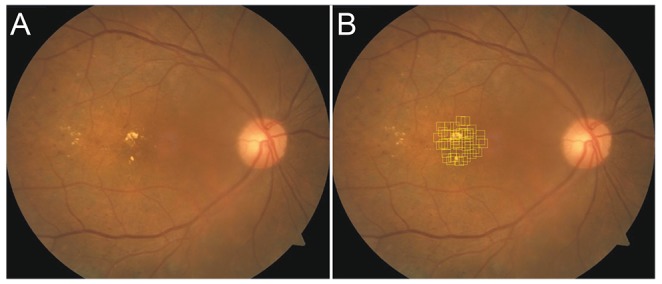
Color fundus photograph of patient's right eye with diabetic macular edema (A). Subthreshold micropulse yellow laser photocoagulation site shown on a color fundus photograph (B). Laser shots were delivered at the same time with a 3 × 3 pattern mode (multiple squares with yellow dashed line) over the entire area of macular edema including the foveal center. Additional laser shots were applied on other edematous retinal areas.
Data were collected in a retrospective fashion from chart reviews and were analyzed using SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA). The post-treatment values were compared with the baseline values using the Wilcoxon signed-rank test with significance corresponding to a p-value of <0.05.
Results
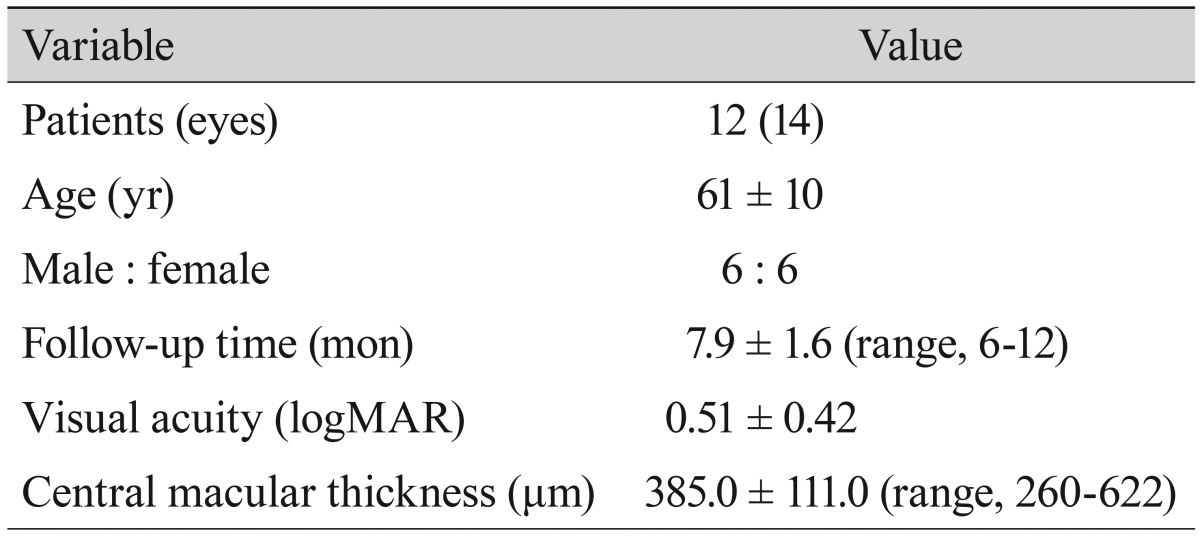
The demographic characteristics and treatment modalities of the patients are shown in Table 1. The mean age of the patients at the time of SMYLP was 61 ± 10 years; an equal number of men and women were included. The follow-up time was 7.9 ± 1.6 months (range, 6 to 14 months). The findings for a 63-year-old woman who underwent successful SMYLP are presented in Fig. 2. Five SMYLP sessions with a different number of laser shots were performed over the course of 12 months. Changes in logMAR VA and CMT values for all eyes are presented on graphs in Fig. 3.
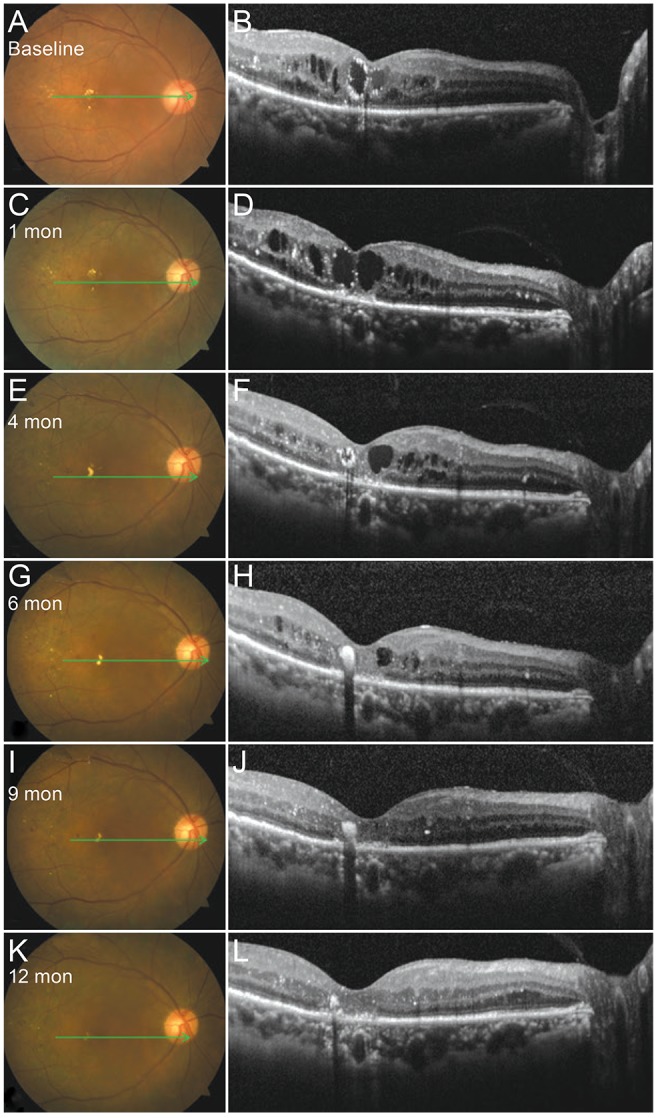
Color fundus photographs and spectral domain optical coherence tomography images of the macula for case 1. The right eye of a 63-year-old woman before (A,B) and after subthreshold micropulse yellow laser photocoagulation (C-L).

Changes in logarithm of the minimum angle of resolution (logMAR) visual acuity (VA) (A) and central macular thickness (CMT) (B).
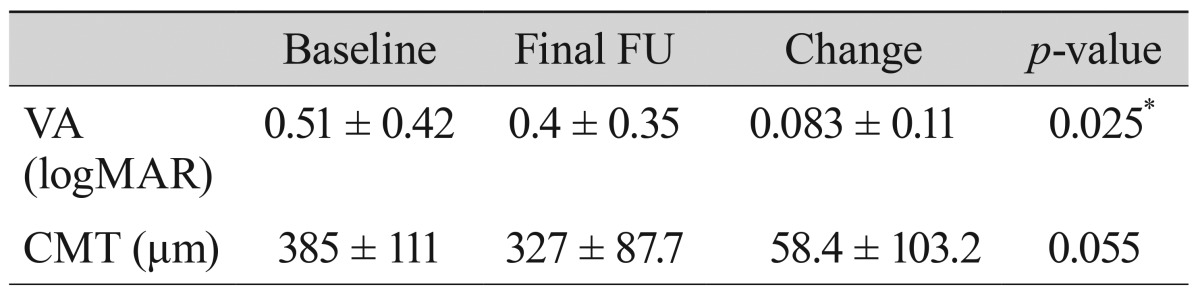
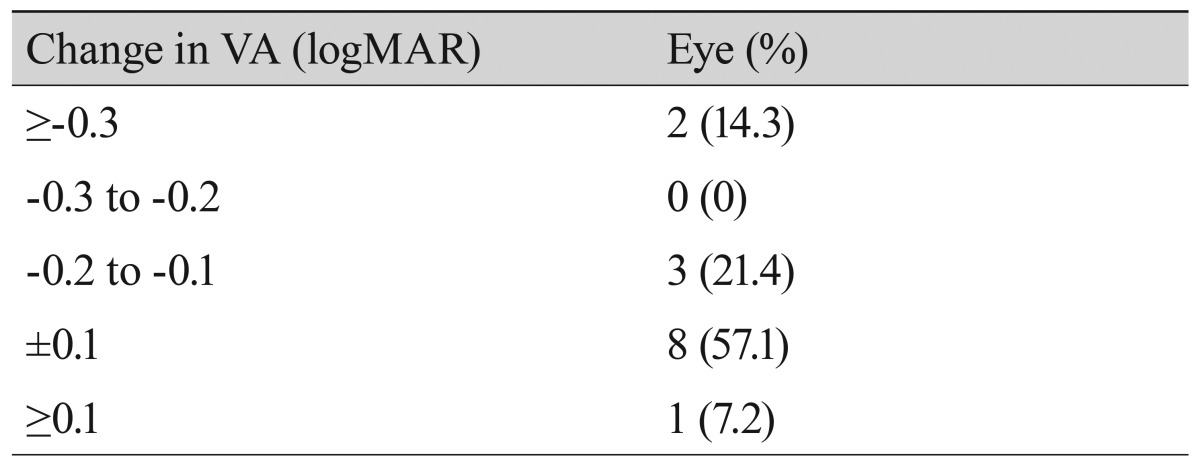
The baseline-corrected VA was 0.51 ± 0.42 logMAR, which improved to 0.40 ± 0.35 logMAR (p = 0.025) at the final follow up (Table 2). At the final follow-up visit, an improvement in VA of >0.3 logMAR was observed in two eyes (14.3%), an improvement of 0.1 to 0.2 logMAR was observed in three eyes (21.4%), eight eyes (57.1%) remained the same, and VA was reduced by >0.1 logMAR in one eye (7.2%) (Table 3).
The CMT was 385.0 ± 111.0 µm at baseline, and the final CMT was 327.0 ± 87.7 (p = 0.055) (Table 2). The mean number of laser shots in one treatment session was 950 ± 499, the mean number of treatment sessions was 3.0 ± 1.2, and the mean number of total laser shots was 3,057 ± 1,518. Six eyes (42.8%) had reductions in CMT of >10% of the baseline thickness, and eight eyes (57.2%) remained the same. The required number of accumulative laser shots required for VA improvement (≥0.1 logMAR) and a reduction in CMT (≥10% of baseline CMT) was 2,140 ± 1,646 (801 to 5,240) and 1,908 ± 1,594 (900 to 5,240), respectively.
When before and after fundus color photographs and autofluorescence images were compared, no laser scars were detected in the color fundus photographs, red-free photographs, or autofluorescence images (Fig. 4). Likewise, no evidence of laser damage was observed by fluorescein angiography, and improved fluorescein leakage was observed after SMYLP in all patients (Fig. 4).

Baseline fundus color photographs, red-free photographs, autofluorescence (AF) and fluorescein angiography (FA) images for (A) case 1; (B) shows images of the same patient 14 months after subthreshold micropulse yellow laser photocoagulation (SMYLP; note the invisible chorioretinal scar in the color photograph, red-free photograph, and AF images, and the reduced fluorescein leakage in the FA image); (C) shows case 2 before treatment and (D) shows images of the same patient six months after SMYLP treatment (note that there is no chorioretinal damage in any of the images and an improved petaloid pattern of hyperfluorescence is observed in the AF and FA images).
Discussion
This study demonstrates that SMYLP improves or maintains VA and CMT in patients with DME. Previous studies [2,17,18,21,22] that have evaluated the effects of micropulse diode laser treatment on DME have reported that it is as effective as the conventional argon laser, and also seems to have some additional advantages. These studies all used an 810-nm diode laser system with different power settings (two-times, three-times, or up to five-times the power of the test burn) and duty cycles (5% to 15%) [21,22,23,24,25]. In addition, they used the modified ETDRS technique with the micropulse instead of CW mode.
Yellow (577 nm) wavelengths are suitable for macular disease as they are absorbed well by melanin and hemoglobin, and only minimally by macular xanthophylls. Although no study has reported large clinical differences related to the wavelength used, the yellow laser may offer some advantages as it is better absorbed by melanin than the 810-nm laser. This property is theoretically suitable for micropulse treatments aimed at RPE cells. The 577-nm wavelength is outside the absorption spectrum of retinal xanthophylls, potentially allowing for treatments close to the fovea. The combined absorption of 577-nm wavelength by melanin and oxyhemoglobin causes lesser scatter compared to green (532-nm) and other yellow (561- to 568-nm) wavelengths. This leads to energy being concentrated in a smaller volume, which in turn allows for a reduction in power and a shortened pulse duration.
To address potential safety concerns, we investigated the effect of repeated subthreshold micropulse laser photocoagulation on the retinas of Dutch belted rabbits in our unpublished study. We varied the repetitions (10, 50, 100, and 200 sessions of micropulse laser photocoagulation), but the 577-nm yellow laser device was used in all of the tests. No obvious laser scars in the treated areas were observed in the rabbit eyes on color fundus and SD-OCT images. Fluorescein angiography did not detect any obvious changes after 10 repetitions, but hyperfluorescence was observed after more than 50 repetitions. There were no changes in histologic findings. We therefore decided to limit the number of repetitions to 10 in our clinical protocol.
We designed a new treatment protocol using one of the pattern modes in the Supra 577Y Laser System. The differences between our new protocol and previous subthreshold laser treatments are outlined below. First, the exposure time during one shot is 20 ms, which is a reduction of 7% to 10%. Increased total laser emission time may result in inadvertent laser delivery, especially in unfixed eyes. Second, to compensate for the reduced exposure time, we increased the number of micropulse shots. Although a considerable number of laser shots are required for this compensation, we gradually increased the number of laser shots from 100 to 2,000 to ensure patient safety. We also determined the effective number of laser shots that did not cause damage in several cases, and we speculated that the appropriate number of laser shots for this protocol would be approximately 2,000. Third, using a pattern mode with repetition made subthreshold laser treatment more comfortable for patients. Previous subthreshold laser treatments may have caused inadvertent chorioretinal damage due to unintended repetition. Another study reported the risk of unintended chorioretinal damage with subthreshold laser treatment, especially when performed by inexperienced physicians, as the laser burn is invisible [2]. Our protocol is safer and more comfortable as it only involves two or three repetitions of very short micropulse laser delivery targeting DME areas, including the fovea. Thus, the risk of inadvertent chorioretinal damage is likely to be lower than in previous subthreshold protocols, and this improved safety profile and greater comfort should enable more physicians to perform subthreshold laser treatments.
Lavinsky et al. [2] reported that results obtained with high-density (HD) subthreshold diode laser micropulse photocoagulation (SDM) with confluent laser application were superior to those obtained with normal density-SDM and mETDRS (determined according to anatomic and functional measures of improvement). Interestingly, the greater functional gain observed in the HD-SDM group was only statistically significant at the 12-month outcome assessment. They hypothesized that progressive healing and usually less scarring due to lighter laser lesions led to better retinal restoration, which could explain the relatively significant late gain of vision [2]. Our findings revealed a discrepancy between two parameters in patients with DME: OCT-measured macular thickness and VA. We hypothesized that visual gain may precede the CMT decrease observed with SMYLP.
Our study shows that SMYLP can have a similar efficacy in DME treatment as conventional laser treatment. Increased efficacy may be achieved by using a wider target area (including the non-edematous retina near the DME lesion) and more compact laser shots than those described for the protocol in the present study. The primary finding of our study is that SMYLP does not cause any chorioretinal damage in the human eye despite repeated micropulse laser treatments (shown by red-free photographs, autofluorescence images, fluorescein angiography, and OCT images). We intend to develop a more effective and safer protocol for SMYLP in the future.
Our study has several limitations. It was a retrospective case series study with an irregular follow-up period and no control group. Therefore, our findings should be interpreted with caution. However, they do provide information for further study. The findings of this study can be summarized as follows: short-term SMYLP is effective and safe; SMYLP can be repeated without chorioretinal damage; SMYLP can be used in areas that include the foveal center; our novel subthreshold treatment protocol utilizing the 577-nm yellow laser system and pattern mode was successfully applied in the treatment of DME. Prospective, randomized, large-scale studies will be required to further evaluate the therapeutic efficacy and safety of this approach and to identify a more effective treatment protocol employing SMYLP.
Notes
No potential conflict of interest relevant to this article was reported.