 |
 |
| Korean J Ophthalmol > Volume 28(4); 2014 > Article |
Abstract
Purpose
To evaluate the changes of higher order aberrations (HOAs) before and after laser subepithelial keratomileusis (LASEK) and to analyze the influence of tear film instability on HOAs of the corneal surface after LASEK.
Methods
In this cross-sectional study, 31 patients who underwent LASEK were divided into dry eye (16 patients, 32 eyes) and non-dry eye groups (15 patients, 30 eyes). Uncorrected distance visual acuity, spherical equivalent refraction, ablation depth, tear film parameters and Ocular Surface Disease Index (OSDI) questionnaire scores were evaluated in both groups. Total HOA root mean square (RMS), third-order coma, third-order trefoil and fourth-order spherical aberration (SA) of the corneal surface immediately and at 10 seconds after blinking were measured before and after surgery.
Results
The total HOA RMS, coma, trefoil and SA significantly increased after LASEK compared with preoperative values in both groups. In the dry eye group, total HOA RMS, coma and trefoil significantly increased except for SA at 10 seconds after blinking compared with those measured immediately after blinking. In addition, the changes of total HOA RMS, coma and trefoil were negatively correlated with tear film break-up time (R = -0.420, -0.473 and -0.439, respectively), but positively correlated with OSDI score (R = 0.433, 0.499 and 0.532, respectively). In the non-dry eye group, there were no significant differences between HOAs measured at 10 seconds after blinking and those measured immediately after blinking.
Laser subepithelial keratomileusis (LASEK) is a laser surgical procedure commonly performed for the correction of refractive errors of the cornea [1]. After a corneal refractive surgery such as LASEK, increased corneal higher order aberrations (HOAs) can contribute to glare, halo, decreased night vision and decreased contrast sensitivity. Also, dry eye is the most common complication after refractive laser procedures including LASEK [2]. Dry eye after corneal surface ablation such as LASEK is attributed to corneal innervation damage, tear film instability, decreased aqueous tear production, corneal and conjunctival epitheliopathy and abnormal distribution of tears on the corneal surface [3,4]. Although post-LASEK dry eye is usually tem porary, some patients have prolonged and severe symptoms such as pain, photophobia, visual fluctuation [5,6]. Furthermore, post-LASEK dry eye may negatively influence patients' satisfaction with the outcome of the procedure.
The precorneal tear film plays an important role in the stability of optical quality of the eye [7,8]. Tear film instability can significantly alter the light pathway and decrease the quality of vision by increasing the ocular aberrations, especially the HOAs [9,10]. Recent studies have assessed temporal wavefront aberrations and the optical effect of the tear film dynamics after blinking [11,12,13]. After blinking, the gradual increase in optical aberrations is associated with an increase of tear film irregularity [14]. Also, numerous studies have shown that the tear film instability in dry eye patients led to wavefront HOA changes [15,16,17,18].
However, little is known about the association between HOAs and tear film instability after corneal refractive surgery. Therefore, the purpose of this study was to evaluate the changes in HOAs before and after LASEK and to analyze the correlations between the changes in HOAs and dye eye parameters for dry eye patients after LASEK.
Our study included patients who received bilateral LASEK for the correction of myopia at the Department of Ophthalmology of the Chonnam National University Hospital from January 2012 to April 2012 and were followed up for at least 6 months after surgery. Exclusion criteria included ocular diseases, previous ocular surgery, punctal plug insertion, abnormality of the nasolacrimal drainage apparatus, eyelid malposition and abnormality of eyelid margin. Informed consent was obtained from all subjects, in accordance with the Declaration of Helsinki, and the protocol was approved by the institutional review board of Chonnam National University Hospital.
Thirty-one patients were divided into 2 groups based on the presence of dry eye. Sixteen patients (32 eyes) had dry eye, and 15 patients (30 eyes) didn't have dry eye. Inclusion criteria for the dry eye group were presence of ocular symptoms, tear film abnormalities (Schirmer I test results <7 mm/5 minutes, tear film break-up time [TBUT] <7 seconds) and ocular surface damage (corneal and conjunctival staining) [19]. All patients were treated with preservative-free sodium hyaluronate 0.1% (Hyalu Mini; Hanmi Pharm, Seoul, Korea). Additionally, topical cyclosporine A 0.05% (Restasis; Allergan, Irvine, CA, USA) was applied twice a day in the patients with dry eye.
All patients underwent ophthalmic examinations including uncorrected distance visual acuity (UDVA) by Snellen chart, spherical equivalent (SE) refraction, ocular surface staining with 1% fluorescein dye, TBUT, Schirmer I test and tear clearance rate (TCR). Ocular surface staining was graded using the Oxford grading scheme (0 to 5): absent (0), minimal (1), mild (2), moderate (3), marked (4), and severe (5) [20]. TBUT, Schirmer I test and TCR were performed as previously described [21]. All examinations were performed by the same researcher. In addition, the Ocular Surface Disease Index (OSDI) questionnaire was done to assess the ocular symptoms and the quality of vision (OSDI score: 0 to 100) [22]. In addition, we evaluated the preoperative SE refraction and ablation depth in all patients.
At 6 months after LASEK, corneal wavefront aberration was measured using the Pentacam (Oculus; Optikgerate GmbH, Wetzlar, Germany). The 'Wavefront Aberration Cornea' data of the Pentacam's Zernike analysis was used. The selected refractive indices were 1.376 and 1.336 for the cornea and the aqueous, respectively [23]. The HOA data were analyzed quantitatively in the central 4-mm pupil diameter up to the sixth order by expanding the set of Zernike polynomials. The Zernike coefficients were viewed in the "|Z| Vectors" presentation mode. The assessed HOA values were total HOA root mean square (RMS), third-order coma, third-order trefoil and fourth-order spherical aberration (SA) of the anterior corneal surface.
All measurements were taken between 10 AM and 4 PM to minimize diurnal changes and performed on 3 separate days (within one week) to yield 3 sets. In addition, the measurements were performed in mesopic condition without any pharmacologic mydriasis [18]. The preoperative HOAs were measured immediately after blinking, while the postoperative HOAs were measured immediately after blinking and at 10 seconds after blinking to evaluate the influence of tear film instability on HOAs of the corneal surface. The patients were instructed to remain stationary and to blink completely just before each measurement. The machine was aligned with the patients' pupillary plane. We used the machine's automatic release mode to eliminate operator-induced errors. Measurements were repeated until a well-aligned and focused image was obtained.
SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA) was used for statistical analyses. Results are presented as mean ┬▒ standard deviation. The chi square test and Mann-Whitney U-test were used to compare the results between the groups. The Wilcoxon signed-rank test was used to compare the intragroup differences. In the dry eye group, Spearman correlation coefficients were used to analyze the association between pairs of variables. A p-value less than 0.05 was considered statistically significant.
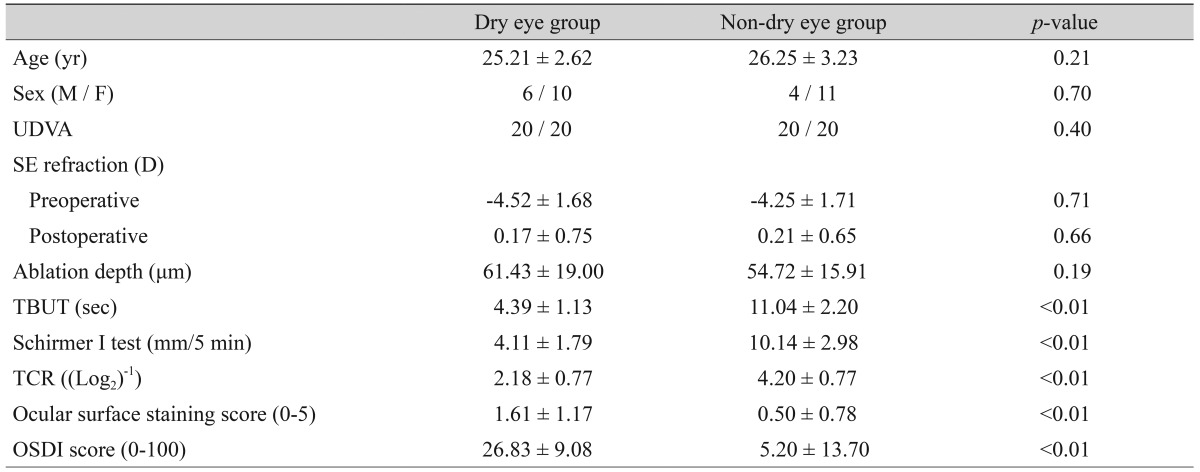
The demographics and characteristics of both group patients are presented in Table 1. In the dry eye group, the mean age of the 6 men and 10 women was 25.21 ┬▒ 2.62 years. In the non-dry eye group, the mean age of the 4 men and 11 women was 26.25 ┬▒ 3.23 years. There were no statistically significant differences in age, sex, UDVA, SE refraction (preoperative and postoperative) and ablation depth between groups. However, there were statistically significant differences in TBUT, Schirmer I test, TCR, ocular surface staining and OSDI scores between groups (p < 0.01). The dry eye group had lower TBUT, Schirmer I test, and TCR scores, and higher ocular surface staining and OSDI scores compared with the non-dry eye group.
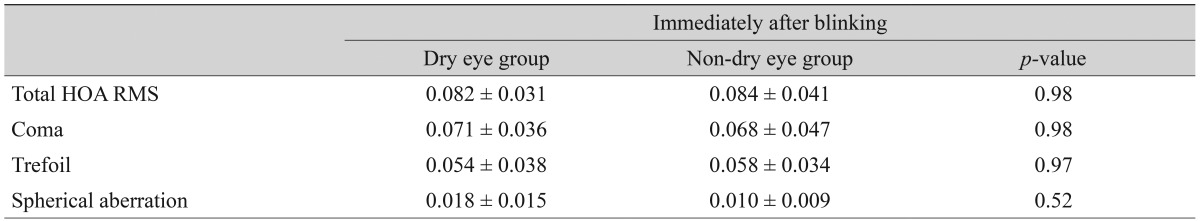
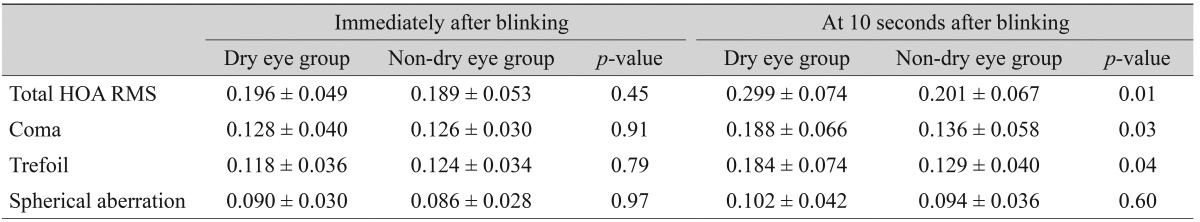
The preoperative and postoperative HOAs of the corneal surface in both groups are presented in Tables 2 and 3. In the dry eye group, the total HOA RMS value was 0.082 ┬▒ 0.031 ┬Ąm preoperatively and 0.196 ┬▒ 0.049 ┬Ąm postoperatively (p < 0.01). Coma, trefoil and SA values were 0.071 ┬▒ 0.036, 0.054 ┬▒ 0.038, and 0.018 ┬▒ 0.015 ┬Ąm preoperatively and 0.128 ┬▒ 0.040, 0.118 ┬▒ 0.036, and 0.090 ┬▒ 0.030 ┬Ąm postoperatively, respectively (p < 0.01 for all). In the non-dry eye group, the respective total HOA RMS, coma, trefoil and SA values were 0.084 ┬▒ 0.041, 0.068 ┬▒ 0.047, 0.058 ┬▒ 0.034, and 0.010 ┬▒ 0.009 ┬Ąm preoperatively and 0.189 ┬▒ 0.053, 0.126 ┬▒ 0.030, 0.124 ┬▒ 0.034, and 0.086 ┬▒ 0.028 ┬Ąm postoperatively (p < 0.01 for all).
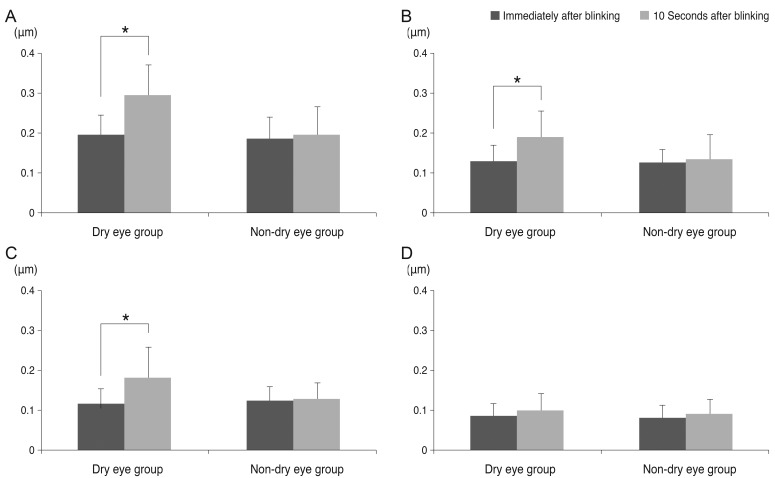
When comparing the dry eye and non-dry eye groups, there were no statistically significant differences in all values measured immediately after blinking before and after LASEK (Tables 2 and 3). However, at 10 seconds after blinking, the dry eye group had significantly higher total HOA RMS (p = 0.01), coma (p = 0.03), and trefoil (p = 0.04) than the non-dry eye group. In the dry eye group, total HOA RMS, coma, and trefoil significantly increased at 10 seconds after blinking compared with those measured immediately after blinking (p < 0.01, p = 0.03, and p = 0.04, respectively), whereas there was no significant difference in SA value (p = 0.62). In the non-dry eye group, there were no statistically significant differences in all HOA parameters (Table 3 and Fig. 1). The mean pupil sizes measured immediately after blinking and at 10 seconds after blinking didn't show significant differences in either group.
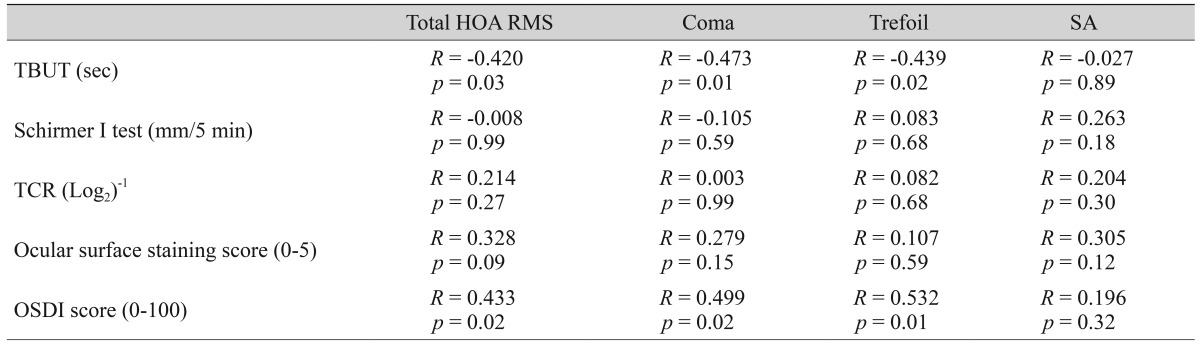
The correlations between the changes in HOAs and dry eye parameters (TBUT, Schirmer I test, TCR, ocular surface staining score, and OSDI score) in the dry eye group are demonstrated in Table 4. The changes of total HOA RMS, coma and trefoil were correlated negatively with TBUT (R = -0.420, p = 0.03; R = -0.473, p = 0.01; R = -0.439, p = 0.02; respectively) but were correlated positively with OSDI score (R = 0.433, p = 0.02; R = 0.499, p = 0.02; R = 0.532, p = 0.01; respectively). Schirmer I test, TCR, and ocular surface staining scores did not show significant correlations with the HOAs.
Optical aberrations result in blurred images and decreased visual quality. Although the HOAs comprise a relatively a lower proportion of optical aberrations than lower order aberrations, they can have an important effect on retinal image quality in subjects [9]. The cornea is the most powerful refractive element of the eye [24]. After corneal refractive surgery, the surgically-induced corneal HOAs can contribute to glare, halo, decreased night vision and decreased contrast sensitivity [25]. As expected, the measured HOAs (total HOA RMS, coma, trefoil, and SA) after LASEK were significantly higher than pre-surgery measurements.
Dry eye is one of the most common complications after refractive surgery. Although the severity is milder than laser in situ keratomileusis, LASEK can also lead to the ocular symptoms associated with dry eye as well as decreased tear secretion [5,6]. After the blinking, a tear meniscus spreads over the entire ocular surface to form a uniform tear film. Then, the tear film gradually thins and breaks up. Tear film instability can lead to disproportionate thickness of the tear film, such as the superoinferior asymmetric contribution or thinning of the central cornea. As a result, tear film irregularity will lead to significant additional aberrations. These abnormal distributions of the tear film on the corneal surface are intensified in patients who received LASEK or patients with dry eye disease.
Some studies demonstrated that tear film instability can cause significantly increased HOAs in patients with dry eye. Montes-Mico et al. [15] reported that dry eye patients showed greater optical aberrations compared with normal controls and that an increase of HOAs resulted from increased tear film irregularity. Koh et al. [17] reported that from 5 to 9 seconds after blinking, the total HOAs were significantly higher than those measured immediately after blinking in subjects with a short TBUT. Denoyer et al. [18] also reported that the RMS of ocular and corneal HOAs, especially third-order aberrations, significantly increased from 6 to 10 seconds after blinking in dry eye patients.
This is the first study, to our knowledge, reporting tear film instability and HOAs after corneal surface ablation. The Pentacam was used to measure the corneal wavefront aberration. It is a noninvasive system using rotating Scheimpflug camera and a monochromatic slit-light source (blue LED at 475 nm) for measuring anterior segment topography [26]. Numerous studies reported that corneal aberrations measured by the Pentacam showed good reproducibility [27,28,29]. Our study showed that total HOA RMS, coma and trefoil significantly increased at 10 seconds after blinking compared with those measured immediately after blinking in dry eye patients after LASEK. This result can be explained by compound effects of corneal shape changes after LASEK and irregular distribution of the tear film by superficial punctuate keratitis, the lid pressure and the gravity effect. On the other hand, there was no statistically significant increase in SA values. Some studies explained that the thinning at the center of the cornea rather than the periphery might contribute to an increase of SA value [17]. Also, the relative contribution of SA to the overall wave aberration of the eye increases when pupil dilates [9]. We believe that several factors may have an influence on the absence of significant changes in SA values in our study. One factor is that there was no definitive pupil size change between the measurement taken immediately after blinking and that at 10 seconds after blinking. Another factor is that the HOAs of the anterior corneal surface might have been affected by the irregular distribution of the tear film rather than thinning of the tear film in the central cornea.
Ridder et al. [30] reported a correlation between the anterior corneal HOAs and subjective assessment of contrast sensitivity. Denoyer et al. [18] reported the progression index for corneal HOAs was correlated with the subjective index (OSDI score) of patient-reported visual outcomes and with objective clinical findings (TBUT). Although there are some differences, such as measurement of HOAs using the Pentacam in dry eye patients after LASEK, our results also showed that the amount of increase in total HOA RMS, coma and trefoil at 10 seconds after blinking compared with those measured immediately after blinking was negatively correlated with TBUT, but positively correlated with OSDI score. We assume that additional HOAs by tear film instability as well as surgically-induced corneal HOAs can lead to a decreased optical quality in dry eye patients after LASEK.
Our study has several limitations. First, because we used the Pentacam to measure the HOAs, we could only assess HOAs of the corneal surface, not whole ocular HOAs. In addition, serial HOAs after blinking were not evaluated. Although optical quality of the actual retinal image is associated with the whole ocular HOAs including the posterior cornea, crystalline lens, and other components of the eye [9], the tear film instability mostly influences aberrations of the anterior corneal surface. Also, corneal aberrations may be correlated with overall ocular aberrations [14]. Second, although we have performed repeated measurements for a well-aligned and focused image, there is a possibility of subtle measurement errors. Third, the sample size is relatively small. Further studies with a larger sample size and serial measurements of corneal and ocular HOAs are needed.
In conclusion, the HOAs after LASEK significantly increased compared with those before surgery. In the dry eye patients after LASEK, the values of total HOA RMS, coma and trefoil at 10 seconds after blinking showed a significant increase compared with those measured immediately after blinking. In addition, the amount of an increase in total HOA RMS, coma and trefoil after blinking was significantly correlated with TBUT and OSDI score. Therefore, the additional HOAs caused by tear film instability in patients after LASEK may lead to a reduction in optical quality.
REFERENCES
1. Azar DT, Ang RT, Lee JB, et al. Laser subepithelial keratomileusis: electron microscopy and visual outcomes of flap photorefractive keratectomy. Curr Opin Ophthalmol 2001;12:323-328.


2. O'Keefe M, Kirwan C. Laser epithelial keratomileusis in 2010: a review. Clin Experiment Ophthalmol 2010;38:183-191.


3. Horwath-Winter J, Vidic B, Schwantzer G, Schmut O. Early changes in corneal sensation, ocular surface integrity, and tear-film function after laser-assisted subepithelial keratectomy. J Cataract Refract Surg 2004;30:2316-2321.


5. Quinto GG, Camacho W, Behrens A. Postrefractive surgery dry eye. Curr Opin Ophthalmol 2008;19:335-341.


6. Ang RT, Dartt DA, Tsubota K. Dry eye after refractive surgery. Curr Opin Ophthalmol 2001;12:318-322.


7. Rieger G. The importance of the precorneal tear film for the quality of optical imaging. Br J Ophthalmol 1992;76:157-158.



8. Tutt R, Bradley A, Begley C, Thibos LN. Optical and visual impact of tear break-up in human eyes. Invest Ophthalmol Vis Sci 2000;41:4117-4123.

9. Lombardo M, Lombardo G. Wave aberration of human eyes and new descriptors of image optical quality and visual performance. J Cataract Refract Surg 2010;36:313-331.


10. Li KY, Yoon G. Changes in aberrations and retinal image quality due to tear film dynamics. Opt Express 2006;14:12552-12559.


12. Montes-Mico R, Alio JL, Munoz G, Charman WN. Temporal changes in optical quality of air-tear film interface at anterior cornea after blink. Invest Ophthalmol Vis Sci 2004;45:1752-1757.


13. Koh S, Maeda N, Hirohara Y, et al. Serial measurements of higher-order aberrations after blinking in normal subjects. Invest Ophthalmol Vis Sci 2006;47:3318-3324.


14. Montes-Mico R, Alio JL, Munoz G, et al. Postblink changes in total and corneal ocular aberrations. Ophthalmology 2004;111:758-767.


15. Montes-Mico R, Caliz A, Alio JL. Wavefront analysis of higher order aberrations in dry eye patients. J Refract Surg 2004;20:243-247.


16. Wang Y, Xu J, Sun X, et al. Dynamic wavefront aberrations and visual acuity in normal and dry eyes. Clin Exp Optom 2009;92:267-273.


17. Koh S, Maeda N, Hori Y, et al. Effects of suppression of blinking on quality of vision in borderline cases of evaporative dry eye. Cornea 2008;27:275-278.


18. Denoyer A, Rabut G, Baudouin C. Tear film aberration dynamics and vision-related quality of life in patients with dry eye disease. Ophthalmology 2012;119:1811-1818.


19. Yoon KC, Im SK, Kim HG, You IC. Usefulness of double vital staining with 1% fluorescein and 1% lissamine green in patients with dry eye syndrome. Cornea 2011;30:972-976.


20. Bron AJ, Evans VE, Smith JA. Grading of corneal and conjunctival staining in the context of other dry eye tests. Cornea 2003;22:640-650.


21. Yoon KC, Park CS, You IC, et al. Expression of CXCL9, -10, -11, and CXCR3 in the tear film and ocular surface of patients with dry eye syndrome. Invest Ophthalmol Vis Sci 2010;51:643-650.



22. Schiffman RM, Christianson MD, Jacobsen G, et al. Reliability and validity of the Ocular Surface Disease Index. Arch Ophthalmol 2000;118:615-621.


23. Oliveira CM, Ferreira A, Franco S. Wavefront analysis and Zernike polynomial decomposition for evaluation of corneal optical quality. J Cataract Refract Surg 2012;38:343-356.


24. Seo KY, Lee JB, Kang JJ, et al. Comparison of higher-order aberrations after LASEK with a 6.0 mm ablation zone and a 6.5 mm ablation zone with blend zone. J Cataract Refract Surg 2004;30:653-657.


25. McAlinden C, Moore JE. Comparison of higher order aberrations after LASIK and LASEK for myopia. J Refract Surg 2010;26:45-51.


26. Shankar H, Taranath D, Santhirathelagan CT, Pesudovs K. Anterior segment biometry with the Pentacam: comprehensive assessment of repeatability of automated measurements. J Cataract Refract Surg 2008;34:103-113.


27. Miranda MA, O'Donnell C, Radhakrishnan H. Repeatability of corneal and ocular aberration measurements and changes in aberrations over one week. Clin Exp Optom 2009;92:253-266.


28. Miranda MA, Radhakrishnan H, O'donnell C. Repeatability of oculus pentacam metrics derived from corneal topography. Cornea 2009;28:657-666.


Fig.┬Ā1
Changes of total higher order aberration root mean square (A), coma (B), trefoil (C) and spherical aberration (D) between values measured immediately after blinking and those measured at 10 seconds after blinking in the dry eye and the non-dry eye groups. *p < 0.05 (comparison of values measured immediately after blinking and those measured at 10 seconds after blinking).
Table┬Ā1
Comparative analysis of demographics and characteristics of patients who underwent laser subepithelial keratomileusis
Table┬Ā2
Comparative analysis of preoperative wavefront HOAs of the corneal surface between the dry eye and the non-dry eye groups after laser subepithelial keratomileusis
Table┬Ā3
Comparative analysis of postoperative wavefront HOAs of the corneal surface between the dry eye and the non-dry eye groups after laser subepithelial keratomileusis



 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print




