Macular holes can be associated with myopia, trauma, scleral buckling, pneumatic retinopexy, and vitrectomy [1,2]. The most commonly accepted theory involves progressive tangential foveal traction against the premacular vitreous cortex [3]. Corneal refractive surgeries have become one of the most globally popular options for the correction of low to moderate myopia. However, vitreoretinal complications, including endophthalmitis, retinal tears, retinal detachment and hemorrhage, have been reported [4,5,6,7]. There are some reports of macular hole formation after laser in situ keratomileusis (LASIK) [8,9,10,11], and one case of unilateral macular hole formation after photorefractive keratectomy (PRK) [8]. In this case report, we describe a case of bilateral macular hole formation after PRK for correction of myopia in a 42-year-old patient.
Case Report
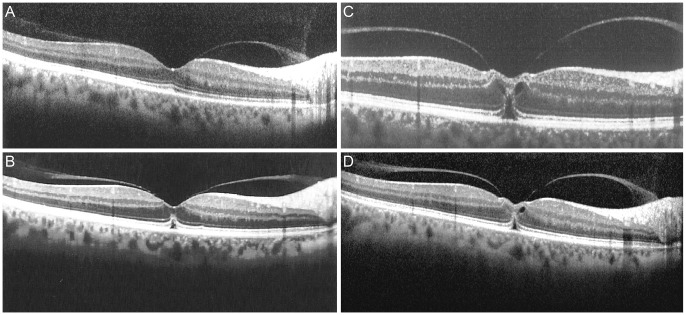
A 42-year-old man who had undergone bilateral PRK two months prior was admitted to our ophthalmology clinic complaining of visual distortion in his left eye. The preoperative best-corrected visual acuity (BCVA) was 20 / 20, and the retinal examination was normal except for peripheral lattice degeneration in both eyes. The preoperative cycloplegic refractive error (spherical equivalent) was -4.5 and -5.0 diopters in the right eye and the left eye, respectively. Post-PRK uncorrected visual acuity was 20 / 20 in both eyes. Two months later, the visual acuity of the left eye had decreased to 20 / 70. Fundoscopy and macular optical coherence tomography (OCT) showed a stage II macular hole of the left eye (Fig. 1A). Simultaneous OCT of the right eye showed vitreous traction on the fovea and mild elevation of the outer retinal layers (Fig. 2A).
One month later, the patient underwent 23-gauge sutureless pars plana vitrectomy (PPV), localized posterior vitreous detachment (PVD) induction in the posterior pole, internal limiting membrane peeling and administration of sulphur hexafluoride gas as a tamponade in the left eye. During the operation, the patient was found to have inferotemporal peripheral lattice degeneration with multiple holes, around which a double line of barrier laser spots was introduced. PVD was not extended to the area of lattice degeneration. By the second postoperative day the macular hole had completely closed. Three weeks later, the SF6 was found to have been resorbed, and the patient's vision had improved to 20 / 40. Indirect ophthalmoscopy revealed an inferotemporal giant retinal tear (GRT) unrelated to the sclerotomies at the site of the previous lattice degeneration but that crossed the laser scars. The patient underwent PPV, endolaser photocoagulation and silicone oil injection. Postoperative examination showed successful retinal reattachment, and his BCVA reached 20 / 70 one month after the final surgery. Macular OCT revealed complete hole closure and restoration of the inner segment/outer segment junction (Fig. 1B). Meanwhile, the patient complained of recent-onset progressive visual distortion in the right eye. At this time (4.5 month after PRK), OCT revealed increased vitreomacular traction and accentuated outer retinal layer distortion compared with the previous OCT, indicating a stage IB macular hole (Fig. 2B). This traction accentuated one week later, and the vision of the right eye was reduced to 20 / 30 (Fig. 2C). However, the degree of traction was decreased three weeks later, the vision in the right eye had improved to 20 / 25 and the posterior vitreous was attached (Fig. 2D). Regular ophthalmic follow-up exams did not show any change over the next two months.
Discussion
Although LASIK and PRK procedures do not involve direct manipulation of intraocular structures, they may induce postoperative vitreoretinal interface changes. Myopia itself is a risk factor for macular hole formation [2]. However, there is not enough data in the literature to determine if these myopic holes would have developed regardless of PRK or if the shock waves generated by the excimer laser may have led to vitreoretinal traction [12].
Arevalo et al. [11] reported a case series of 20 eyes with a full-thickness macular hole after LASIK. One of the patients in their study showed bilateral involvement. The mean time interval between LASIK surgery and macular hole formation was 12 months, and the mean age was 46 years.
Chan and Lawrence [8] reported a series of three eyes of three myopic patients who developed a macular hole in an eye after bilateral LASIK or PRK. After PRK surgery in a 45-year-old white man, a stage II macular hole developed nine months after refractive surgery for -7.0 diopters of myopia.
Ruiz-Moreno et al. [9] reported a case of a macular hole developing in a myopic eye after LASIK. Vitreofoveal traction occurring after LASIK seems to be the predominant force in hole formation. The acute intraocular pressure increase associated with the mechanical stretching induced by the suction ring, as well as the shock waves generated by the excimer laser may lead to vitreomacular traction after LASIK [12].
Although myopia itself is a risk factor for macular hole formation, the short interval between refractive surgery and macular hole formation, bilateral involvement and the moderate myopic refractive error in this case highlight the possible role of PRK in macular hole formation.
This patient developed a GRT after primary vitrectomy for the macular hole that developed at the site of pre-existing lattice degeneration and atrophic holes despite the use of a barrier laser. This break was not sclerotomy-site related. PVD induction during primary vitrectomy was not extended to the lattice area, so the remaining vitreous cortex may have contracted and progressed enough to cause significant vitreoretinal traction. This may explain the GRT formation that bypassed the barrier lasered lattice degeneration.
To our knowledge, this case is the first report of bilateral macular hole formation following PRK. Vitreous surgery of the first eye necessitated by macular hole surgery resulted in a very early postoperative inferior retinal giant tear, which could be explained by the additive effect of vitreous detachment from vitrectomy surgical manipulation.
The myopic refractive error in our patient was in the moderate range (less than 6 diopters), highlighting the possible effect of PRK on the development of the retinal pathologies we encountered. The accelerated nature of the PVD in the right eye documented by serial OCT imaging could explain these complications.
An important limitation of this study is that, owing to its retrospective nature, OCT was not performed before PRK. Although a causal relationship between PRK and macular hole formation has not yet been established, it is recommended to add PRK to the list of surgical procedures that may be associated with macular hole formation. Future prospective investigations might be valuable for determining the vitreoretinal interface changes that occur after PRK and to help identify other predisposing risk factors for macular hole formation.




 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print






