Infants under one year of age have various ocular disorders ranging from refractive errors to retinal abnormalities. Among these diseases, some such as conjunctivitis, keratitis, and corneal abrasions are treatable with medication; however, other diseases, such as infantile esotropia, congenital cataract, congenital glaucoma, and retinal problems require early surgical treatment to prevent further deterioration [1]. Many of the causes of blindness are also avoidable, as they are either preventable or treatable in childhood [2].
Despite the importance of early diagnosis of childhood diseases, cooperation between the guardian and physician is one of the key factors affecting the ability to formulate a correct diagnosis. As a result, pediatricians or primary ophthalmologists can make incorrect diagnoses owing to the lack of guardian cooperation. Therefore, to present the basic outline of diagnoses based on symptoms, we investigated the chief complaints and ocular disorders in infants under one year of age and analyzed the association between the complaint and disorder.
Materials and Methods
A total of 815 infants (400 boys and 415 girls) visited the outpatient clinic of Kim's Eye Hospital between July 2011 and May 2012 and were under one year of age. We retrospectively reviewed the charts of these 815 infants. Chief complaints were obtained from guardians, including the patients' father, mother, or grandparents and they were categorized into the following 11 categories: eyelid drooping, epiphora (tearing), ocular discharge, lid swelling, eyelashes touching the eyeball, abnormalities of the anterior segment, abnormal eyeball movement (e.g., squint or nystagmus), red eye, trauma, poor eye contact, and miscellaneous. Abnormalities in the anterior segments included leukocoria, spot or foreign body in the cornea, conjunctiva and sclera, and iris problems, such as color difference between the two eyes. Lastly, miscellaneous complaints included the following: blinking, eye rubbing, photophobia, and a foreign object in the eye. Congenital nasolacrimal duct obstruction (CNLDO) was defined as a patient with high tear meniscus height and mucopurulent reflux from the punctum when gentle pressure was applied over the lacrimal sac. Conjunctivitis was classified into three types (epidemic keratoconjunctivitis, allergic conjunctivitis and unspecified conjunctivitis).
We performed ophthalmologic examinations, such as manifest refraction, the Brückner test, a fundus examination, and an alternate cover test at the clinicians' discretion. We tried to group all complaints into the 11 categories and we made a diagnosis using objective methods. This research study was reviewed and approved by the institutional review board of Kim's Eye Hospital.
Results
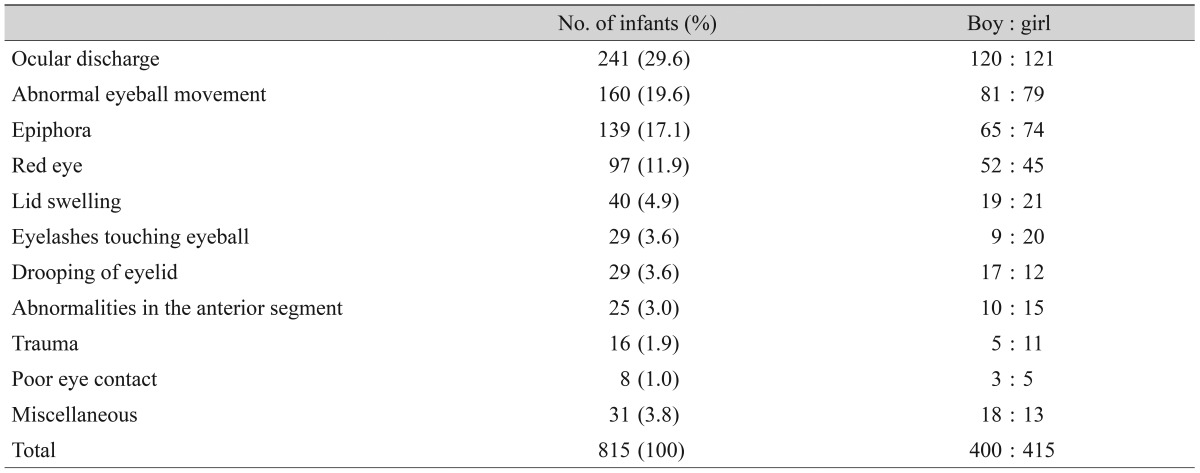
The mean age of the infants seen at the outpatient clinic was 6.09 ± 3.07 months. The most common chief complaint was ocular discharge followed by abnormal eyeball movement, epiphora, and eye redness (Table 1).
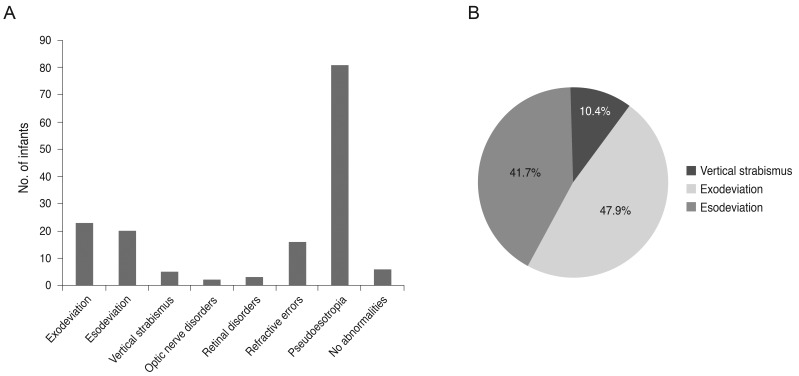
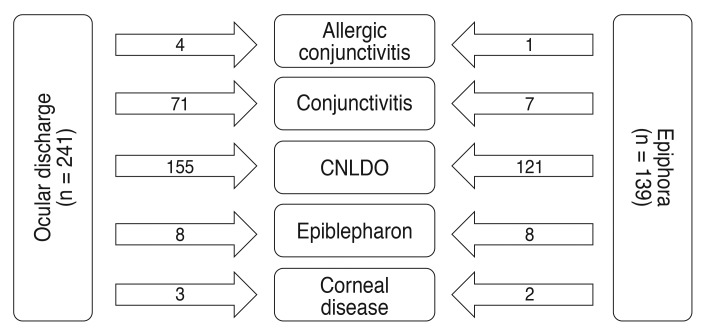
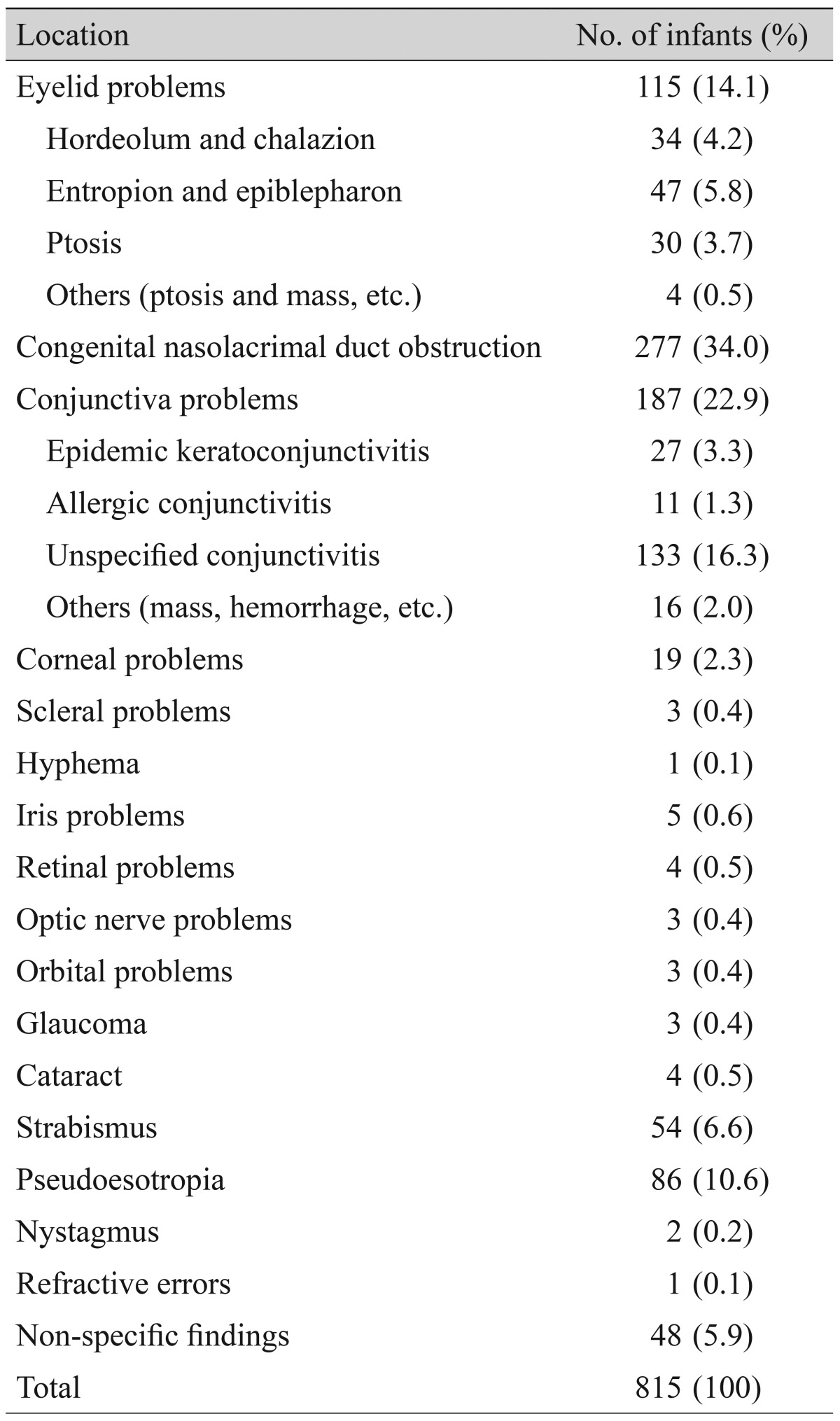
Among infants with ocular discharge, most were afflicted with CNLDO (155 infants) and conjunctivitis (75 infants). A total of 160 guardian complained of abnormal eyeball movement and 86 of these 160 infants (51.9%) were diagnosed with pseudoesotropia. Of all infants, exodeviation was found in 17.9% and esodeviation was found in 16.4% (Fig. 1). The majority of infants with epiphora had confirmed cases of CNLDO (84.3%, 119 of 141), eight had epiblepharon, seven had conjunctivitis, and seven were due to other causes. Two-thirds of the infants with red eye was due to various types of conjunctivitis, including viral or allergic causes. Among conjunctivitis, allergic conjunctivitis occurred in 11 infants and epidemic keratoconjunctivitis was diagnosed in 27 infants. The majority of eyelid mass lesions (27 of 40) were hordeolum or chalazion. All infants who presented with guardian complaints of drooping eyelids were afflicted with true blepharoptosis. In the 16 infants with a history of trauma, corneal erosions caused the trauma in six of them, subconjunctival hemorrhages in three, and orbital contusion in two. Five infants had normal findings. Epiphora and ocular discharge were common symptoms in infants, which were accurate reflections of the diagnosis (Fig. 2). The two infants with nystagumus (0.24%) had congenital nystagmus (Table 2).
There were eight complaints of poor eye contact in infants and the diagnoses in these cases consisted of three retinal disorders, two congenital optic nerve disorders, one cataract, one glaucoma, and one high hyperopia. Table 3 shows the characteristics of vision-threatening disorders including glaucoma, cataract, corneal ulcer, retinal disorders, and optic nerve disorders.
Discussion
In the current study, we found that the most common symptom in infants under one year of age was ocular discharge followed by abnormal eyeball movement, epiphora, and eye redness.
The main cause of ocular discharge in our patients was CNLDO. Our results showed that the guardians of about 56% of CNLDO infants complained of ocular discharge and 44% complained of epiphora. Global incidence of CNLDO is widely distributed from 1.2% to 20% [3,4]. Spontaneous remission occurs throughout the year and in 96% of these infants, the condition resolves before the age of 1 [4]. CNLDO may include various symptoms such as epiphora, increased tear lake, and discharge [5]. Holmes et al. [6] developed a questionnaire for CNLDO assessing symptoms including tearing, redness of the eyeball, and eye rubbing and their results attest to the questionnaire's usefulness for evaluating CNLDO. Ocular discharge and epiphora are frequently identical and some guardian confuse the two symptoms. Infants with epiphora are a common problem and several diseases, including epiblepharon, conjunctivitis, and CNLDO can result in epiphora [4]. Guez and Dureau [7] reported that the main causes of tearing are CNLDO and congenital glaucoma, the latter accounting for the seriousness of this condition. Corneal abrasions are also extremely common among 1- to 12-week-old infants and have unclear clinical significance [8]. We found that 2 of 139 cases of infant epiphora were due to corneal abrasions.
Redness of the eye is a common symptom and Ubah et al. [9] reported that the most frequent cause of red eye was trauma in 48 (41.0%) patients, followed by allergic conjunctivitis in 29 (24.8%). However, the most common cause of red eye in the present study was conjunctivitis. This difference may be attributable to age difference because Ubha's study evaluated people of all ages.
Although a study in Singapore reported that the prevalence of exotropia exceeded esotropia by a ratio of 7 : 1 [10], the current study documented that exodeviation and esodeviation occurred in similar proportions (exodeviation, 47.9%; esodeviation, 41.7%). In the exotropia cases, the majority of infants suffered from intermittent exotropia [11]. Intermittent exotropia develops between the ages of 10 months and 4 years; however, it can be difficult to detect in its early stages [12]. Thus, this may be why exodeviation and esodeviation had a similar prevalence in our study. Of infants initially diagnosed with pseudoesotropia under the age of 3, 10% are later found to have strabismus, including 15 with esodeviation, three with exodeviation, one with Duane syndrome, and one with Prader-Willi syndrome and esotropia [13]. Thus, we should evaluate pseudoesotropia in infant carefully.
Rapoport et al. [14] reported that eye injuries in children up to 5 years of age were more common in boys (135 boys and 66 girls) and the frequent types of eye injuries were perforation of the cornea and/or sclera, corneal erosion, and hyphema. The present study showed that girls were more susceptible to eye injury; hyphema was noted only in one child and the most common pattern observed was corneal erosion (6 of 16 children). Again, this discrepancy may be attributable to the different ages of children enrolled in these studies. We found retinal problems in 11 of our 815 patients (1.3%). When we suspected retinal problems, we performed restrictive fundus examinations. Therefore, the actual prevalence of retinal problems might have been higher than we observed.
Vision-threatening disorders such as congenital cataracts, congenital glaucoma, corneal ulcer, and Leber's congenital amaurosis should be detected as soon as possible. Congenital cataracts are treatable and we can prevent amblyopia with surgical treatment. The incidence of congenital cataracts varies from 1 to 3 / 10,000 live births or 10 per million of the total population in low-income countries [15]. Although the present study was designed using infants who visited the eye hospital, cataracts were noted in the 0.5% of infants and three of four (75%) presented with guardian complaints of leukocoria. Three infants had congenital glaucoma and the main symptom was corneal haziness. Seidman et al. [16] reported that 32% of congenital glaucoma cases had the full spectrum of classic symptom complex, including epiphora, photophobia, and blepharospasm and 21% of infants and children presented with guardian having noted signs of infantile glaucoma without the child ever reporting symptoms.
The study has some limitations. First, the present study noted a low incidence of refractive errors because we did not perform refraction in all patients. Thus, if we had investigated refractive errors in all infants, the actual incidence of refractive errors may have been higher. Second, infants were evaluated by several ophthalmologists and thus, selected examinations were performed depending on the guardian's chief complaint. As a result, other problems could have been missed.
In conclusion, the most common symptoms in infants under one year of age were usually mild symptoms such as ocular discharge, epiphora, and eye redness. However, infants with poor eye contact or suspected abnormal eye movement should be considered for full ophthalmologic examinations.




 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print






