Graded Decompression of Orbital Fat and Wall in Patients with Graves' Orbitopathy
Article information
Abstract
Purpose
To investigate the results of graded decompression of orbital fat and walls in Graves' orbitopathy (GO) considering the degree of proptosis reduction at surgery and preoperative computed tomography (CT) findings.
Methods
This is a retrospective interventional case series. Graded orbital fat and wall decompression was performed in 90 orbits of 55 patients. In patients with enlarged extraocular muscles and minimal orbital fat proliferation in preoperative CT scans, one- or two-wall decompression of posterior orbit was performed with minimal fat excision. In other cases, the maximal amount of fat tissue was removed from the post-septal area to the apex. If the proptosis was not satisfactorily symmetrically reduced at surgery, one- or two-wall decompression was performed successively. Symmetric reduction of proptosis was consistently confirmed intraoperatively to assure that a desired amount of exophthalmos reduction was achieved.
Results
Four types of decompression were performed: fat only (group 1), fat and one-wall (group 2), fat and two-wall (group 3), and two-wall and minimal fat decompression (group 4). The mean preoperative Hertel value (20.6 ± 2.8 mm) was reduced significantly at six months postoperatively (16.1 ± 2.3 mm). Proptosis significantly decreased with a mean of 4.3 ± 1.7 mm, and the reduction was greatest (5.1 ± 2.1 mm) in group 3. In group 1, a significant correlation between Hertel change and the volume of resected orbital fat was found (r = 0.479). Diplopia was newly developed or aggravated postoperatively in eight patients, and six of these patients were in group 3. With the exception of one patient, visual acuity improved to nearly normal postoperatively in all patients with optic neuropathy.
Conclusions
Graded orbital decompression of orbital fat and bony walls, as assessed by the degree of proptosis reduction during surgery, was effective and predictable with minimal complications in GO patients with vision-threatening or cosmetically disfiguring proptosis.
Graves' disease is an autoimmune disease of the thyroid gland that activates gland function, leading to excessive production of thyroid hormones. Up to 50% of patients with Graves' disease present with pathological features in the eye, known as Graves' orbitopathy (GO) [1-3]. The most common manifestations of GO include upper eyelid retraction, edema, erythema of periorbital tissues, and proptosis. Approximately 3% to 5% of individuals with GO suffer from intense pain and inflammation, diplopia, and vision-threatening compressive optic neuropathy.
The well-established treatments for GO are systemic immunosuppression with glucocorticoids, external beam radiotherapy, and surgery, including orbital decompression and corrective surgery for eyelid retraction and restrictive myopathy [4]. Indications for orbital decompression include optic neuropathy, persistent inflammation or congestion refractory to steroid treatment, and the desire to reduce excess proptosis. Recently, the indications for surgery have increased to include not only optic neuropathy or severe proptosis causing exposure keratopathy, but also cosmetic disfigurement [5]. As surgical indications expand, preoperative conditions have diversified, and there is a need to adjust surgical methods on an individual basis. Several types of orbital decompression have been described, including combinations of lateral wall, medial wall, floor, and orbital fat decompression [6-8].
Several studies have investigated the effect of graded orbital bony decompression through various approaches to achieve the desired effect in proptosis reduction with minimal induced diplopia [5,9-13]. Orbital fat decompression techniques have been reported to offer significant reduction in proptosis in fat-predominant GO patients, with a low complication rate [14,15]. Kikkawa et al. [9] reported a graded orbital decompression based on preoperative exophthalmos. Recently, balanced medial and lateral wall decompression with or without orbital fat decompression has been reported to be effective in reducing proptosis, postoperative diplopia, and postoperative hypoglobus [11,16,17]. Surgeons must decide whether or how to remove orbital bony wall(s) and fat, as well as the amount and location of fat and/or bone removal.
In our experience, the amount of fat removed during surgery or the reductive effect of removing the same amount of fat cannot be completely predicted by preoperative computed tomography (CT) scans or exophthalmos alone but can be predicted according to the state of orbital adipose tissue fibers or the stiffness of extraocular muscles. Thus, the surgical method can be adapted intraoperatively according to the degree of proptosis reduction and the degree of muscle enlargement on preoperative CT scan. The purpose of this study was to investigate surgical outcomes of graded decompression of orbital fat and bony wall(s) by intraoperative evaluations of proptosis reduction.
Materials and Methods
Patients
A consecutive group of patients undergoing orbital decompression for GO between January 2009 and June 2012 was studied retrospectively. Data were obtained from the electronic medical records of Severance Hospital, Yonsei University College of Medicine, Seoul, Korea. All surgery was performed by one surgeon (JSY). Patients with at least six months of follow-up after surgery were recruited. The present retrospective study was approved by the Ethics Committee of Yonsei University College of Medicine, Seoul, Korea.
Preoperative examinations included complete ophthalmic evaluations with best-corrected visual acuity (BCVA), Hertel exophthalmometry (Carl Zeiss, Jena, Germany), intraocular pressure, HESS screening, and Goldmann binocular single vision (BSV) test to assess the range of extraocular muscle motility and diplopia. Preoperative orbital CT was obtained for all patients to evaluate the degree of extraocular muscle or orbital fat enlargement and evidence of a crowding apex. Postoperative assessments were performed one week and one, three, and six months after surgery. Particular attention was paid to preoperative and postoperative Hertel values (six months after surgery).
Myopathy scoring was obtained from all patients before and after surgery. All patients were scored from 3 to 0 (3 = primary diplopia or no orthotropia at the primary position, 2 = orthotropia at the primary position, but with diplopia within 30° in BSV or more than 10° limitation in HESS, 1 = diplopia only outside 30° in BSV, 0 = no diplopia at any gaze).
Indications for orbital decompression included compressive optic neuropathy or persistent congestion refractory to steroid treatment and the desire to reduce excess proptosis for cosmetic improvement. In cases of cosmetically disfiguring proptosis, we preoperatively confirmed clinically metabolically inactive disease status of the patient for at least six months.
Surgical technique
In patients presenting with enlargement of extraocular muscles and minimal to no orbital fat proliferation in preoperative CT scans, the posterior part of one wall (ethmoid bone) or two walls (ethmoid bone and orbital floor medial to the infraorbital nerve complex involving the posterior strut) were removed with minimal fat excision (less than 1 mL) (Fig. 1). However, in cases with fat volume enlargement shown in CT scans, decompression of fat alone or in combination with one or two bony walls, was accomplished through a combined canthofornix and caruncular approach according to the reduction of proptosis during surgery (Fig. 1). All patients with optic nerve compression required two-wall decompression, with or without fat removal.

Algorithm of the surgical approach for orbital fat and/or bony decompression according to preoperative computed tomography (CT) scans in patients with Graves' orbitopathy. When preoperative CT scans showed significant extraocular muscle (EOM) enlargement with minimal fat proliferation, posterior one-wall (ethmoid) or two-wall (combined with orbital floor, including the posterior strut) decompression was performed without fat removal or with minimal fat removal (less than 1 mL). However, if increased orbital fat volume was primarily observed, rather than EOM enlargement shown in CT scans, the maximal amount of extraconal fat tissue was removed from the inferotemporal area, towards the medial orbit, with conservative removal of intraconal fat tissues. If proptosis was not sufficiently and symmetrically reduced during surgery, a one-wall or two-wall decompression was added successively until sufficient reduction of proptosis was achieved.
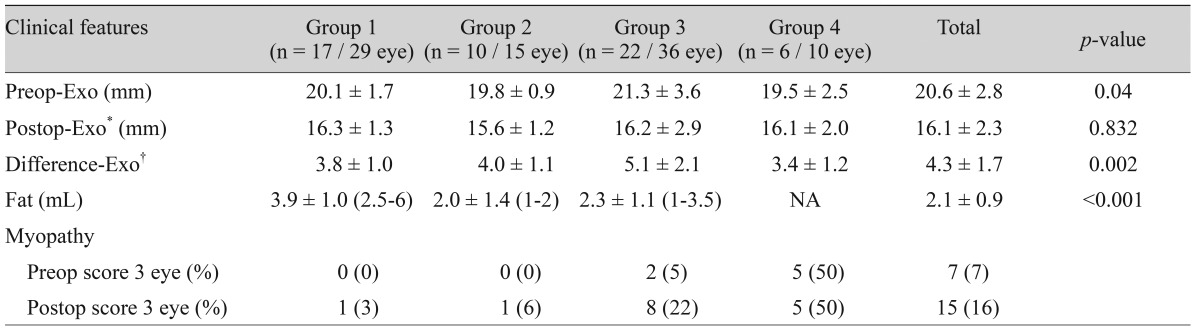
Under general anesthesia, the operation was performed through a swinging eyelid approach. After incision, the orbital septum was visualized all the way caudal to the arcus marginalis. Intraoperative photographs of fat removal are shown in Fig. 2. All post-septal medial, central, and lateral fat pads were excised after septal incision. Extraconal adipose tissues were carefully removed with cutting and cautery. For further fat removal, intermuscular connective tissues and muscle-periorbital septa were dissected. Since the inferotemporal pocket between the lateral and inferior rectus muscles has the largest amount of fat and is relatively safe to dissect, fat was removed until the surfaces of the inferior oblique muscle and inferior rectus muscle were clearly visible and was further resected immediately proximal to the anterior end of the inferior ophthalmic fissure (Fig. 2B and 2D). In the inferomedial space, the septa was incised to remove fat, but care was taken to avoid the insertion site of the inferior oblique muscle (Fig. 2B and 2D), and the fat medial to the medial rectus muscle was removed through a transcaruncular approach. Superomedial fat was additionally removed by incising the intermuscular septum above the medial rectus muscle. In this way, the maximum amount of orbital fat could be removed while sparing only the superotemporal fat around the lacrimal gland and superior fat tissues. For further decompression, the deep and posterior loose intraconal fat was carefully removed using forceps and scissors as necessary. The volume of removed fat was measured using a 10-mL syringe.
Intraoperative photographs showing fat removal method. After removal of the post-septal medial, central, and lateral fat pads, maximal amounts of caruncular (A), inferolateral and inferomedial fat tissues (B) were removed through transcaruncle and canthofornix incision after careful dissection of intermuscular septa without damaging the medial, inferior rectus muscle (IR) and inferior oblique (IO) muscle. (C,D) Fat was removed until the surface of the IO muscle, and inferior and medial rectus muscle (MR) were clearly visible, and was further resected immediately proximal to the anterior end of the inferior ophthalmic fissure. Superomedial fat was additionally removed by incising the intermuscular septum above the MR, and for further decompression, the deep and posterior loose intraconal fat was carefully removed until satisfactory reduction of proptosis was achieved using forceps and scissors conservatively. Severe exophthalmos (E) was significantly reduced (F) by the removal of orbital fat. The level of corneal apex became lower than the eyelids. *Deep posterior intraconal fat.
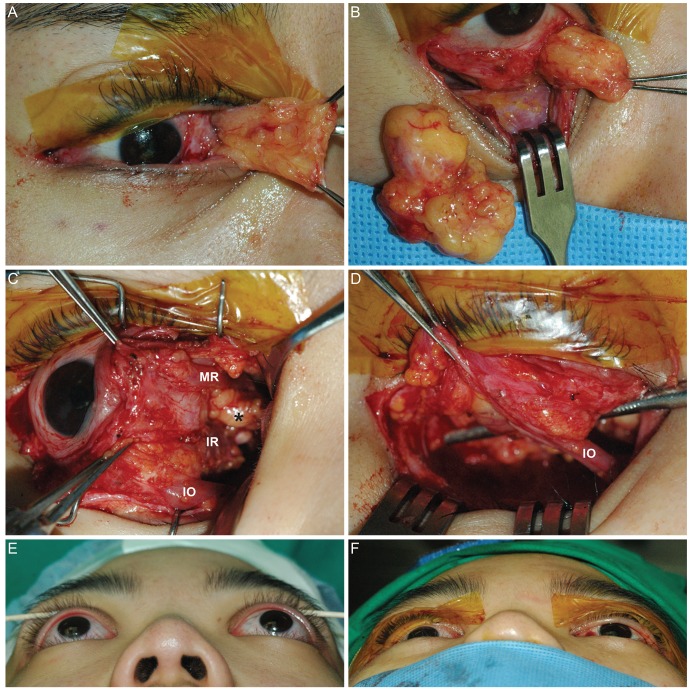
During surgery, symmetric reduction of proptosis was intraoperatively confirmed by one surgeon. The height of the cornea apex was measured with a ruler from the level of the bony edge of the zygoma at the lateral canthus by looking parallel to the plane of the patient's eye from the side. Symmetry was verified by looking down from the patient's head with the eyes at the same level as the frontal bone, to assure that the desired amount of exophthalmos reduction (mm) was achieved (Fig. 3A and 3B). If fat decompression alone was insufficient for proptosis reduction, a transcaruncular orbital decompression of the posterior ethmoid bone was then performed (Fig. 3A and 3B). If exophthalmos was still significant or not symmetrical, the posterior part of the orbital floor was decompressed, mostly involving the posterior strut, as shown in Fig. 3C and 3D. A Barovac (Cardinal Health, Dublin, OH, USA) drain was inserted through a stab skin incision at the inferior orbital rim to prevent postoperative retrobulbar bleeding. The conjunctiva was closed using 6-0 absorbable Vicryl sutures. Intravenous methylprednisolone (250 mg for one day) and oral prednisolone (20 mg daily for two weeks and then 15 mg daily for two weeks) were given postoperatively.
Intraoperative photographs showing adjustment of the decompression method according to intraoperative assessment of proptosis reduction (A) By Hertel exophthalmometry, 22.5 and 24 mm of exophthalmos in the right and left eyes, respectively were measured before surgery. (B) After the removal of the maximal amount of fat (right, 4.8 mL OD; left, 3.8 mL OS) in both eyes, satisfactory reduction of proptosis was achieved in the right eye through fat-only decompression. However, a posterior two-wall decompression was further performed in the left eye to achieve a sufficient proptosis reduction. Finally, the level of cornea apex became lower as much as desired amount of decompression with symmetry. (C) Preoperative computed tomography (CT) scans (axial, coronal, and sagittal views) shows significant increases in fat volume without extraocular muscle involvement. (D) Postoperative CT scans (axial, coronal, and sagittal views) show significantly decreased volumes of extraconal and intraconal fat tissues, especially at the inferior orbit in both eyes.
Statistical analyses
SPSS ver. 18.0 (SPSS Inc., Chicago, IL, USA) was used. Paired t-test, ANOVA with Bonferroni correction, and Pearson's chi-squared test were used to compare demographics and postoperative outcomes between different surgical groups. Pearson correlation and linear regression analysis were performed to correlate the resected amount of fat and postoperative Hertel change. The results were considered statistically significant if p-value was less than 0.05.
Results
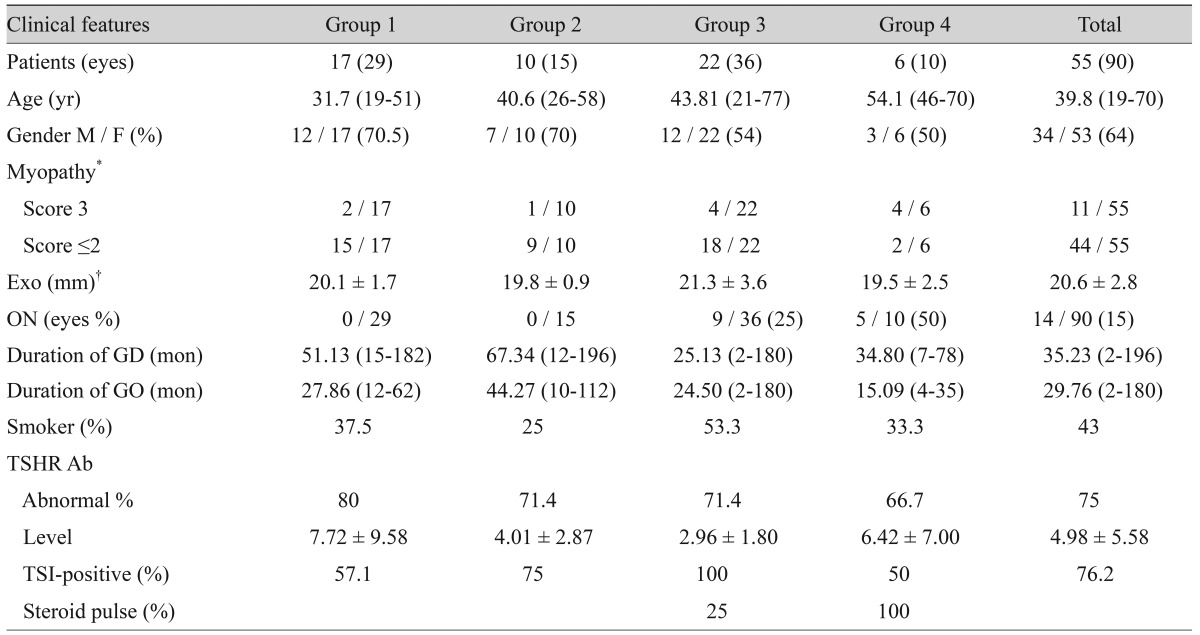
In total, 55 patients (90 orbits) who underwent graded orbital decompression with at least six months of postoperative follow-up were recruited. We grouped eyes according to the type of surgery performed and according to the amount of fat and the number of decompressed orbital bone(s) (Table 1). Fat-only decompression (group 1), fat and one-wall decompression (group 2), fat and two-wall decompression (group 3), and two-wall decompression with minimal fat (<1 mL) (group 4) was performed in 29 eyes (17 patients), 15 eyes (10 patients), 36 eyes (22 patients), and 10 eyes (6 patients), respectively. Table 1 shows preoperative demographic and clinical characteristics.
In preoperative CT scans, ten eyes showed significant enlargement of extraocular muscles with minimal to no orbital fat proliferation. These cases presented with vision-threatening optic neuropathy with apical crowding as shown in CT scans (five eyes) or severe congestion refractory to steroid treatment (five eyes). In these cases, two-wall decompression with posterior strut removal was performed with minimal fat excision (group 4).
In the other 80 eyes, a considerable amount of fat decompression, with or without bony wall removal, was performed (groups 1 to 3). In 49 eyes (54%), there was fat volume enlargement without muscle involvement shown in preoperative CT scans (25 eyes in group 1 [86%], 15 eyes in group 2 [100%], and 13 eyes in group 3 [36%]).
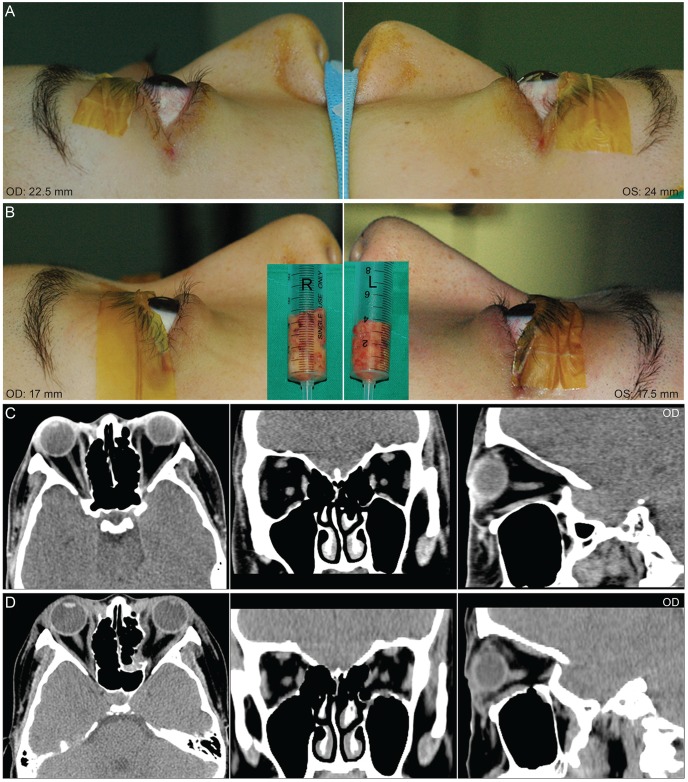
There were 14 eyes with compressive optic neuropathy. All underwent two-wall decompression with minimal (n = 5, group 4) or significant (n = 9, group 3) removal of orbital fat tissues, as shown in Fig 4. With the exception of one patient who had preoperative visual acuity of hand motion in one eye due to prolonged compression, preoperative BCVA (all less than 40 / 200 on a Snellen chart with relative afferent pupillary defect [RAPD]) significantly improved postoperatively to nearly normal vision without RAPD.

Preoperative and postoperative photographs and computed tomography (CT) scans in a 70-year-old female patient with compressive optic neuropathy, proptosis, restrictive myopathy, and congestion due to Graves' orbitopathy, who underwent orbital fat and posterior two-wall decompression. (A) Preoperative photographs and CT scans. Red dotted line indicates the outline of fat removal. (B) Postoperative photographs and CT scans at 6 months after surgery. Congestive symptoms and signs including chemosis, conjunctival injection, caruncular swelling, and lid erythema and swelling all resolved after surgery. Compressive optic neuropathy was also completely resolved.
The mean preoperative Hertel values (20.6 ± 2.8 mm) were significantly reduced at six months after surgery (16.1 ± 2.3 mm, p < 0.05) (Table 2). Mean preoperative exophthalmos was greatest in group 3 (21.3 ± 3.6 mm, p = 0.04); however, no difference was found in postoperative Hertel values between groups (p = 0.832). Proptosis significantly decreased with a mean of 4.3 ± 1.7 mm, and the reduction was greatest (5.1 ± 2.1 mm, p = 0.002) in group 3.
The mean amount of fat removed during surgery was 2.1 ± 0.9 mL in 80 eyes of groups 1 to 3 (Table 2). The amount of fat removed was greatest in group 1 (3.9 ± 1.0 mL; range, 2.5 to 6; p < 0.001), where we found a significant correlation between Hertel change and the volume of resected orbital fat with a correlation coefficient of 0.479 (p = 0.009). Linear regression revealed the following equation: 0.481 × resected fat volume (mL) + 2.456. However, the average Hertel change versus resected orbital fat volume was approximately 1 (3.8 / 3.9).
With respect to diplopia, seven patients reported diplopia at primary gaze, scoring 3 with significant restriction of motility both before as well as after surgery. In eight additional patients, six of whom were included in group 3, the myopathy score increased from 2 to 3 (Table 2). Twelve patients reported clinically insignificant diplopia outside 30° in BSV after surgery, requiring no further surgical treatment.
All patients exhibited insignificant hypoesthesia in the lower cheek area, but all resolved after six months postoperatively. Otherwise, no significant intraoperative or postoperative complications developed.
Discussion
GO can be categorized into fat-, muscle-, or inflammatory-dominant, or more frequently, combined type. Many variations in orbital decompression have been introduced for treatment of this condition [7,18-21]. The amount of proptosis reduction has been reported to be associated with the number of walls removed [6], the number and size of cuts made in the periorbita [22], and the type of preoperative proptosis [23]. However, because many complex factors influence the amount of proptosis reduction, it is difficult to predict postoperative outcomes of decompression [11,18,23-25]. To date, thyroid orbital surgeons have developed their own surgical procedures to best predict favorable surgical outcomes. In this study, we present our postoperative results after combined graded fat and bony wall decompression, adjusted by intraoperative assessment of proptosis reduction. Symmetric reduction of proptosis and desired amount of decompression were consistently measured and confirmed by one surgeon during surgery. In our study, proptosis decreased to a mean of 4.3 ± 1.7 mm, and there was no significant difference in postoperative exophthalmos between the groups, although preoperative exophthalmos differed in each group. A mean of 3.8 mm and 5.1 mm of proptosis reduction was observed in patients who underwent fat only removal (3.9 ± 1.0 mL) and combined fat and two-wall decompression (2.3 ± 1.1 mL), respectively.
As previous studies reported, GO has a complicated pathogenesis and differs in each case. There is no single, all-purpose method of treatment or evaluation [14,15,26-28]. With repeated surgery, clinicians can develop their own standardized intraoperative evaluation methods. Posterior medial and floor decompression surgery is a traditional technique. Using the results of preoperative CT analysis, we decided to perform two bony wall decompressions in cases with predominantly muscle-enlarged orbits with minimal to no fat proliferation, and minimal to no fat (less than 1 mL) was removed, as anticipated. In cases with more than moderately enlarged fat tissues, prolapsing extraconal and intraconal fat tissues were first removed, and conservative deep and posterior intraconal fat excision was performed with special care via the transcanthoforniceal and caruncle swinging eyelid approach. We cannot completely preoperatively predict the required amount of fat removal or the number and position of bone removal for sufficient proptosis removal based only on CT scan and exophthalmos since the characteristics of GO orbital tissues are largely heterogeneous with respect to fibrotic nature. The effect of decompression can be far weaker in patients with more fibrotic orbital tissues, which cannot be predicted before surgery. Therefore, by intraoperative evaluation of proptosis reduction, we successively performed bony wall decompression involving the posterior ethmoid, with or without the posteroinferior wall and posterior strut. This surgical step was quite effective for cosmetic improvement and minimized new onset of diplopia after surgery.
Proptosis reduction by fat removal is reported to range from 1.8 to 4.4 mm, which is comparable to bony decompression [24,28-32]. After fat only removal in 29 eyes of our cases, a significant correlation was found between Hertel change and the volume of resected orbital fat. The equation determined by linear regression was 0.481 × resected fat volume (mL) + 2.456, which was similar to a recent report [24]. In that report, the mean Hertel change was 4.1 mm with a mean of 4.4 mL fat resection in 44 orbits from 22 patients. However, the ratio of average Hertel change to resected orbital fat volume was approximately 1 in our cases, similar to the report by Liao and Huang [24], indicating a discrepancy between the linear regression result and the averages. This discrepant result is believed to be due to either a resistance to decompression due to different levels of tissue fibrosis among the patients or inclusion of pre-equatorial fat in the linear regression formula, which could not significantly reduce proptosis.
To reduce the incidence of postoperative diplopia, several surgical techniques including balanced orbital decompression [7,10], deep lateral wall decompression [33,34], prevention of the anterior periorbita [35], and intraconal fat removal [29,30,36] have been reported. However, there is no surgical standard to date. Induced diplopia after orbital decompression has been reported to be present in up to 64% of patients [6]. Nunery et al. [37] reported that seven of 14 (50%) Nunery type II patients without preoperative primary-position diplopia had primary diplopia after orbital inferomedial two-wall decompression. In our study, seven patients had preoperative primary diplopia. Diplopia was aggravated postoperatively in eight patients (14.5%), and six of the eight patients were included in group 3, one in group 1, and one in group 2. All 15 patients with a postoperative myopathy score of 3 had preoperative diplopia within 30 degrees of the central field and significant restriction of motility.
Fat decompression may take more time than bone only decompression with regard to bleeding control and minimization of damage to structures around muscles. However, fat decompression has many advantages over other decompression types including preservation of the orbital walls and thus a lower incidence of surgically-induced diplopia. Since fat decompression is not associated with bone removal, the potential for side effects, such as infraorbital nerve hypoesthesia, cerebrospinal fluid leak, and diplopia, are at least theoretically minimized [24,31]. Garrity [38] reported that the diplopia seen in association with fat decompression seemed to be different from the diplopia associated with bony decompression in that the disrupted intermuscular septa might cause more extensive restriction and be more difficult to repair than that seen with bony decompressions.
Until approximately postoperative 1 to 3 months, patients in the present study complained of diplopia, which might be associated with a transient hypoglobus caused by massive removal of the inferior half of the orbital fat tissues and the bleeding or edema around muscles related to the disruption of intermuscular septa. However, all patients showed significant improvement of diplopia and ocular motility within six months. There was only one patient in the fat-only removal group, a 65-year-old male who was a heavy smoker, who developed increased limitation of motion after the operation, as assessed by HESS, and increased diplopia using BSV. He had a history of chronic maxillary and ethmoid sinusitis, which was still present in preoperative CT scan, although he underwent endoscopic sinus surgery before decompression. In preoperative evaluation, right medial rectus muscle enlargement and spontaneous break of the right ethmoid bone were observed on CT scan. We performed fat decompression, with 6.5 mL taken from the right orbit and 6 mL taken from the left orbit, and a break in the posterior ethmoid was found intraoperatively. Exophthalmos decreased from 23 mm OD, 22 mm OS to 16 mm OD, 15 mm OS, and clinical activity score decreased from 6 to 1 postoperatively. A previous study reported that chronic sinusitis can worsen GO status [36]. Worsening of diplopia after fat decompression in this case might have been related to sinusitis or spontaneous bone decompression due to muscle enlargement.
Additional lateral orbital wall removal was not necessary in any patients included in this study. We assume the reason was that the amount of bone removal could be decreased after maximal orbital fat removal, or the clinical characteristics of GO either in Asian patients or just in patients included in the study were not severe enough to require three-wall decompression. The mean preoperative exophthalmos (±SD) was 20.6 ± 2.8 mm. Asian GO patients tend to demonstrate less severe proptosis or myopathy than Caucasians [39] and thus may require less aggressive wall decompression. Sasim et al. [40] reported that an approximately 5.6 mm reduction of proptosis was achieved by medial, floor, and lateral bony wall decompression. However, the conservative bone expansion and intraconal fat removal using suction cutting only produced a mean of 2.4 mm of proptosis reduction [41], suggesting that more aggressive removal of bones could produce further reduction of proptosis.
A study recently reported that the long-term effect of unilateral orbital fat decompression for the reduction of proptosis may be weak, leading to regression [42], whereas wall decompression has characteristics largely opposite to those of fat decompression. In one case of a 45-year-old female, proptosis slightly progressed six months postoperatively. Her preoperative exophthalmos was measured as 20 mm in both eyes, preoperative clinical activity score was zero, and the duration of GO was 30 months. The patient underwent orbital one-wall compression with fat removal in both eyes for cosmetically disfiguring proptosis. After six months of surgery, exophthalmos was 16.5 mm in both eyes without any signs of inflammation. However, the patient complained of regression of proptosis, with exophthalmos measured as 18 mm at eight months after surgery in both eyes. However, no sign of orbital inflammation was found, and thyroid hormone levels were within normal range. Two years postoperatively, exophthalmos stabilized as 17 mm in both eyes. Other than this case, there were no cases of proptosis regression observed in the present study; however, we could not compare results with patients who underwent surgery with no adjustment due to the retrospective nature of this study. further long-term follow-up study might be necessary to verify this phenomenon.
In conclusion, maximal amounts of extraconal and intraconal fat excision with conservative removal of deep posterior intraconal fat, combined with traditional one- or two-posterior bony wall decompression based on intraoperative assessment of proptosis reduction can be an effective and safe surgical method.
Notes
No potential conflict of interest relevant to this article was reported.