Laser vision correction has been widely used for surgical correction of refractive error since refractive surgery was first reported by the Columbian ophthalmologist Barraquer in the early 1960s. Several studies have demonstrated the efficacy and safety of this procedure [1-3]. Manifest refraction and visual acuity using the Snellen chart have frequently been employed to evaluate the clinical outcomes of these techniques [1-3]. However, measurement of visual acuity using the Snellen chart is subjective and thus may not reflect the true visual quality [4]. For this reason, there have been several attempts to objectively evaluate visual acuity and quality. In the past decade, several studies have measured visual outcome after ophthalmic surgery using various parameters, including higher-order aberrations (HOAs) [5-8]. Unfortunately, aberrometers cannot detect scattering, which limits the extent to which they can estimate objective optical quality. The lens array within an aberrometer removes the effect of scattering. Therefore, the actual scattering cannot be detected, and the optical quality can thus be overestimated when scattered light predominates [9].
Other parameters used to assess optical quality are the modulation transfer function (MTF) and Strehl ratio. Several studies have shown these parameters to provide a valid evaluation of optical quality [10-12], however, the MTF and Strehl ratio are difficult to measure under clinical conditions. In recent years, the double-pass technique has been shown to be a useful tool for measuring the effects of both HOAs and scattering [13,14]. The double-pass technique allows the assessment of retinal image quality using a point source object in a near-infrared laser diode (780 nm). The point source object is projected into the eye, and the image is recorded and analyzed after reflection on the retina through the ocular media [13]. The patient's spherical refractive error cannot affect the retinal image quality because it is corrected automatically by the double-pass system device. However, the cylindrical refractive error has to be corrected with an external lens. The double-pass technique can provide retinal image quality as we can set up desired pupil diameter. One commercially available device based on the double-pass technique is the Optical Quality Analysis System II (OQAS II; Visiometrics SL, Terrassa, Spain). The OQAS II measures several parameters that estimate optical quality, including the MTF, Strehl ratio and objective scatter index (OSI) [15-17]. The OSI represents the amount of scattered light.
Only a few published studies have compared optical quality before and after laser vision correction. Ondategui and associates evaluated optical quality using a double-pass system preoperatively and three months after photorefractive keratectomy (PRK) or laser in situ keratomileusis (LASIK) [18]. Their results suggested that optical quality was reduced after PRK and LASIK, with no significant differences between the two surgical techniques.
To our knowledge, there has been no serial follow-up study to measure the optical quality after PRK or LASIK. Therefore, this study has two objectives. The first is to confirm the results of the previous double-pass system-based study. Second, we wish to evaluate the optical quality after PRK or LASIK to follow the recovery of several parameters of optical quality, including the MTF, Strehl ratio, and OSI.
Materials and Methods
Study design
This prospective observational case study evaluated retinal image quality before and after LASIK or PRK. The inclusion criteria were mild to moderate myopia (spherical equivalent ≤-6.00 diopters [D]), stable myopia for the previous year before surgery, and normal intraocular pressure with range of 10 to 21 mmHg. Patients with anterior segment disease, astigmatism greater than 2.00 D, abnormal corneal topography or an abnormal posterior pole evaluation were excluded. All patients had surgery at HanGil Eye Hospital, Incheon, Korea, between September 1, 2011, and November 30, 2011.
The study conformed to the tenets of the Declaration of Helsinki, and was approved by the hospital's Ethics Committee. All patients provided fully adequate signed informed consent to participate.
Surgical technique
All of the surgeries were performed by the same surgeon (THL). The Wave Eye-Q laser system (Alcon, Fort Worth, TX, USA) was used with wavefront optimized treatment, a 6.5 mm optical zone a nd a standard 9.0 mm transition zone for all LASIK surgeries. The flap was created with the Visumax femtosecond laser system (Carl Zeiss Meditec, Jena, Germany) at 110 µm thickness and 8 mm diameter. Postoperatively, moxifloxacin hydrochloride 0.5% (Vigamox, Alcon) was prescribed four times a day for one week, and artificial tears were prescribed every two hours. Prednisolone 1% (PredForte; Allergan, Irvine, CA, USA) was prescribed four times a day for the first postoperative week, and then fluorometholone 0.1% (Flumetholon; Santen, Osaka, Japan) was prescribed four times a day for the next three weeks.
PRK was also performed using the Wave Eye-Q laser system with the same profile treatment, a 6.5 mm optical zone and a standard 9.0 mm transition zone. Before ablation, the epithelial layer was removed with a brush (Amoils epithelial scrubber; Innovative Excimer Solutions, Toronto, Canada). Mitomycin C was then applied to the stromal bed for 12 seconds. After surgery, a bandage contact lens was applied and left in place for one week. Patients received moxifloxacin hydrochloride 0.5% (Vigamox, Alcon) four times a day for one week. Fluorometholone 0.1% (Flumetholon, Santen) was prescribed four times a day for one month with the dose tapered over the next two months.
Patient evaluation
The surgical outcomes were evaluated by measuring corrected distance visual acuity (CDVA), uncorrected distance visual acuity (UDVA), manifest refraction, and optical quality. In the LASIK group, the outcome parameters were assessed preoperatively, and one day, one week, one month, and three months after surgery. In the PRK group, the patients were evaluated preoperatively and one and three months postoperatively. Optical quality was evaluated using OQAS II with the artificial pupil diameter set to 4 mm. One drop of artificial tears was instilled before each double-pass measurement in order to reduce the influence of dryness on the ocular surface. During the measurements, spherical refractive error was automatically corrected by the double-pass system, but cylindrical error had to be corrected manually using the external lens. As proper use of the OQAS II requires some skill, the most experienced optometrist handled the instrument. The optical quality was assessed twice using the OQAS II, and the better results were used for analysis.
Statistical analysis
Statistical analysis was performed using the SPSS ver. 17.0 (SPSS Inc., Chicago, IL, USA). Paired t-tests were used to compare between preoperative and postoperative parameters within both the LASIK and PRK groups. Independent t-tests were used to compare the results between the surgical techniques.
Results
This consecutive prospective serial case study comprised 51 eyes of 35 patients who underwent LASIK and 57 eyes of 37 patients who underwent PRK (Table 1). The age, sphere, cylinder and spherical equivalent did not differ between the surgical groups, suggesting that their preoperative parameters were comparable.
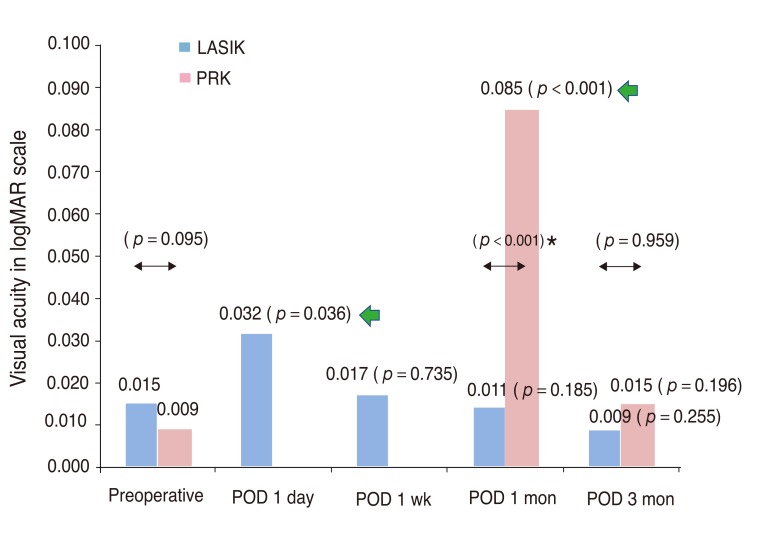
Visual acuity
We measured the preoperative CDVA and postoperative UDVA using the logarithm of minimum angle resolution (logMAR) scale (Fig. 1). The mean preoperative CDVA measurements were 0.015 in the LASIK group and 0.009 in t he PRK group, while t he mean measurements t hree months after surgery were 0.009 in the LASIK group and 0.015 in the PRK group. In the LASIK group, the postoperative day 1 UDVA was significantly different from the preoperative CDVA (p = 0.036), but the later results were not (p = 0.735 after one week, p = 0.185 after one month, p = 0.225 after three months). However, in the PRK group, the one month postoperative UDVA was still significantly different from the preoperative CDVA (p < 0.001), although this difference had disappeared by three months after surgery (p = 0.196). The visual acuity at one month differed significantly between the surgical techniques (p < 0.001), but the three month result did not (p = 0.959) (Fig. 1).
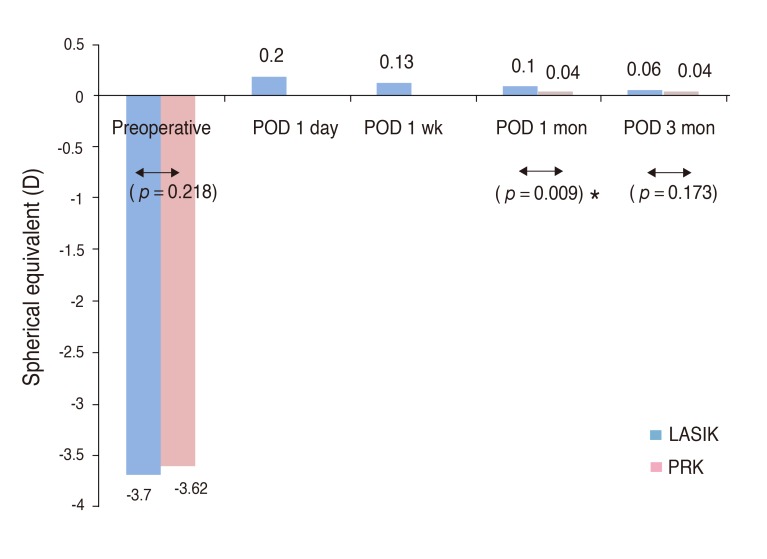
Spherical equivalent
The manifest refraction spherical equivalents measured preoperatively and postoperatively are shown in Fig. 2. The spherical equivalents at three months after surgery were 0.06 in the LASIK group and 0.04 in the PRK group. The spherical equivalents differed significantly between the surgical groups one month after surgery (p = 0.009), at which time the PRK group result was closer to emmetropia (0.04 D [PRK] vs. 0.10 D [LASIK]), but they no longer differed significantly three months after surgery (p = 0.173).
Modulation transfer function cutoff value
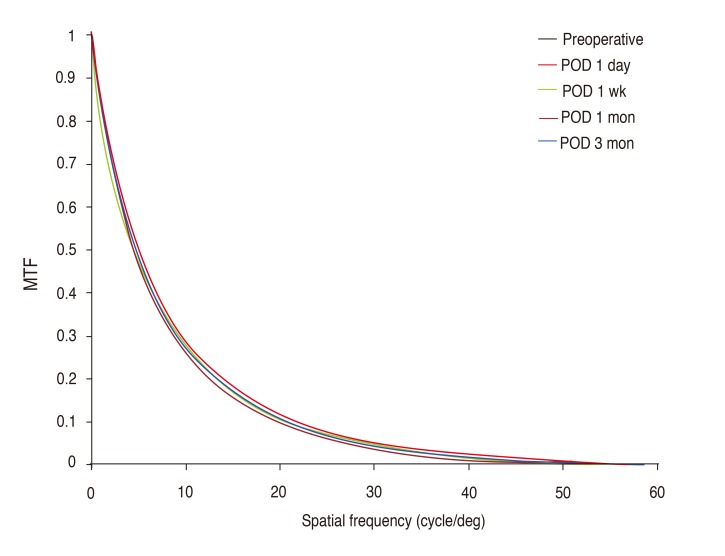
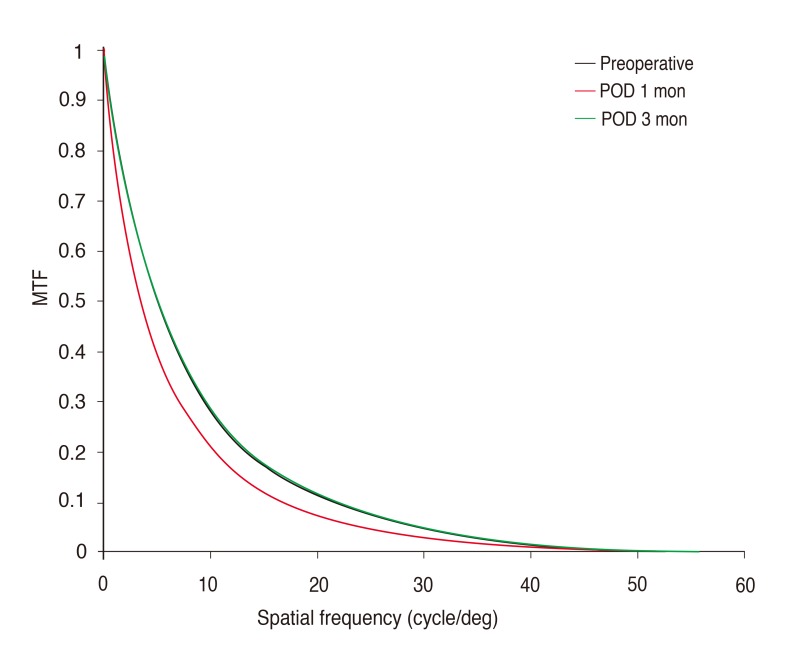
The preoperative and postoperative MTF cutoff values are shown in Fig. 3. The mean preoperative MTF cutoff values were 44.72 in the LASIK group and 43.97 in the PRK group, while the mean measurements three months after surgery were 44.55 in the LASIK group and 43.36 in the PRK group.
In the LASIK group, the MTF cutoff value measured one day after surgery was significantly different from the preoperative value (p = 0.031,) but the later results were not (p = 0.323 after one week, p = 0.929 after one month, p = 0.659 after three months). However, in the PRK group, the MTF cutoff one month after the surgery was significantly different from the preoperative value (p < 0.001), although this difference had disappeared by three months after surgery (p = 0.196). The MTF cutoff values one month after surgery differed significantly between the two surgical technique groups (p < 0.001), but the three-month results did not (p = 0.438) (Fig. 3).
Plotting the mean preoperative and postoperative MTF results of each group as a function of the spatial frequency (Figs. 4 and 5) showed that the retinal image quality worsened until one day after surgery in the LASIK group and one month after surgery in the PRK group. However, the later results show almost complete recovery one week after surgery in the LASIK group and three months after surgery in the PRK group.
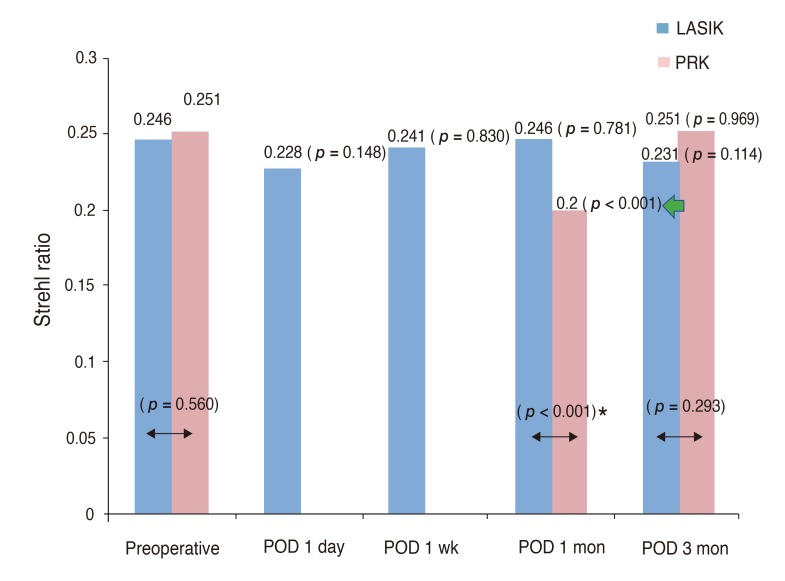
Strehl ratio
The preoperative and postoperative Strehl ratios are shown in Fig. 6. The mean preoperative Strehl ratios were 0.246 in the LASIK group and 0.253 in the PRK group, and the mean measurements three months after surgery were 0.231 in the LASIK group and 0.251 in the PRK group. The preoperative and postoperative Strehl ratios did not differ significantly in the LASIK group. However, the results in the PRK group were similar to those for the visual acuity and the MTF cutoff value. The results one month after surgery differed significantly between the surgical technique groups (p < 0.001), while the three-month results did not (p = 0.293).
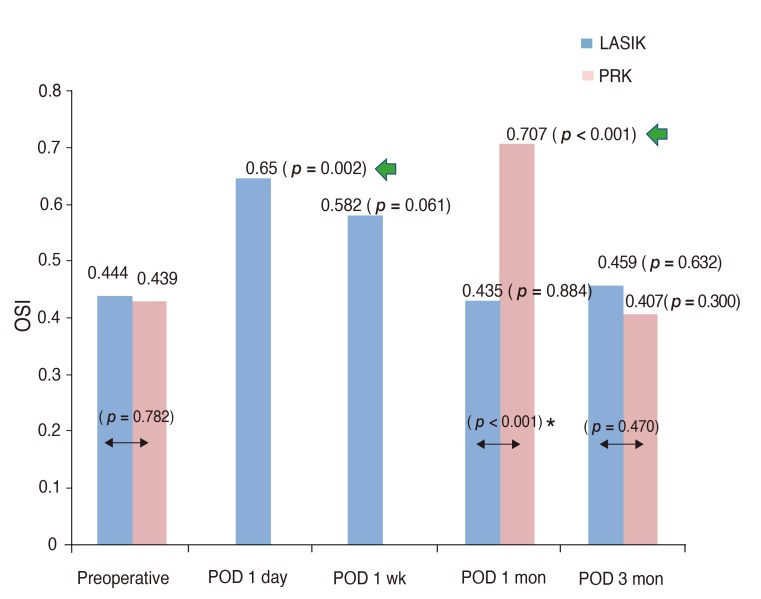
Objective scatter index
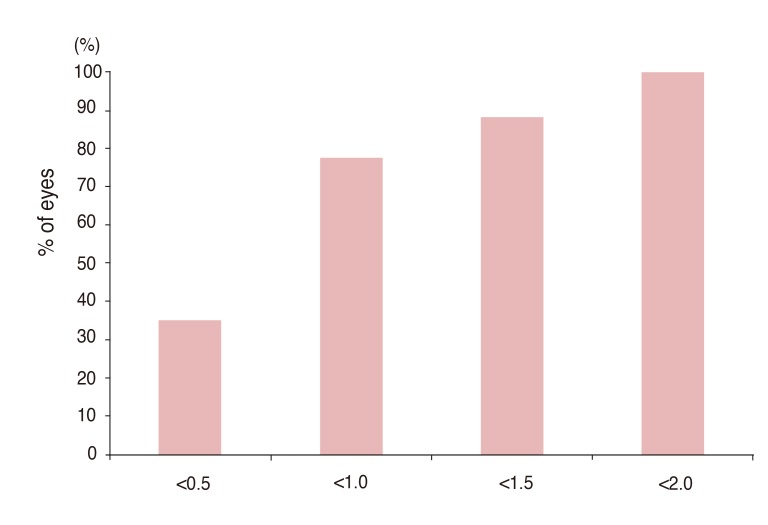
The preoperative and postoperative OSI measurements are shown in Fig. 7. The OSI results of both groups were similar to those for the visual acuity and the MTF cutoff value. The mean preoperative OSI was 0.44 in both groups, and the mean postoperative measurements three months after surgery were 0.046 in the LASIK group and 0.041 in the PRK group. The surgical technique groups differed one month (p < 0.001) but not three months (p = 0.470) after surgery. The UDVA one month after PRK was greater than 20 / 25 (logMAR <0.1) in 56% of patients who noticed no visual problems in daily life. By contrast, the OSI one month after PRK was less than 0.5, the preoperative average (0.439), in only 35% of patients (Figs. 8 and 9).
Discussion
Several studies have reported excellent visual acuity results after laser vision correction [2,3,19,20]. However, measurements of visual acuity alone do not necessarily reflect optical quality, so there have been several attempts to objectively evaluate optical quality. The double-pass technique has been shown to accurately estimate the eye's optical quality [9]. This method records and analyzes images from a point-source object after reflection off of the retina and a double pass through the ocular media. The OQAS II is the only commercially available device based on the double-pass technique. The OQAS II measures several optical quality parameters, including the MTF, Strehl ratio, and OSI. The first of these, the MTF, evaluates the ratio as a function of the spatial frequency between the original contrast and the contrast sensitivity function produced by the eye's optics including the contrast degradation. If there is no contrast degradation, as in a perfect optical system, the contrast in the image will be the same as the contrast in the object, and the highest MTF value will be recorded [16]. In the double-pass system, the MTF cutoff value refers to the frequency up to which the eye's optics can image an object on the retina with a 1% contrast, corresponding to an MTF value of 0.01. Physically, it is assumed that 30 cycles per degree corresponds to 20 / 20 Snellen acuity [16,21].
The Strehl ratio is the ratio of the peak diffraction intensities of a measured eye to those of an aberration-free eye. It is computed as the ratio of the volume under the MTF curve of the patient's eye to that of a perfect wavefront [16,21]. This provides overall information on the optical quality. A Strehl ratio of 1 indicates an ideal optical system limited only by diffraction [16].
The OSI represents the amount of intraocular scattered light and is calculated as the ratio of the amount of the light recorded between 12 and 20 arcmin to that recorded in a 1 arcmin radius from the center [22]. The higher the OSI value, the higher the amount of intraocular scattering [16]. The OQAS user manual says the OSI value is lower than 0.5 in normal young eyes, between 1.5 and 4.0 in eyes developing a cataract, and higher than 4 in eyes with a mature cataract.
Our results suggest that recovery of optical quality after laser vision correction occurs within one week after LASIK but requires between one month and three months after PRK. In the LASIK group, the postoperative day 1 MTF cutoff value and OSI were significantly different from the preoperative values (MTF cutoff value, p = 0.031; OSI, p = 0.002). However, one week after surgery, the MTF cutoff value and OSI were no longer significantly different from the preoperative values (MTF cutoff value, p = 0.323; OSI, p = 0.061). None of the postoperative Strehl ratio measurements differed significantly from the preoperative value (p = 0.148 after one day, p = 0.323 after one week, p = 0.781 after one month, and p = 0.114 after three months). In the PRK group, the MTF cutoff value, Strehl ratio, and OSI measured one month after PRK were significantly different from the preoperative values (p < 0.001 for all parameters), but the three-month results were not (MTF cutoff value, p = 0.602; Strehl ratio, p = 0.969; OSI, p = 0.300).
Three months after laser vision correction, the LASIK and PRK groups did not differ significantly in postoperative visual acuity (0.009 [logMAR] in the LASIK group vs. 0.015 [logMAR] in the PRK group, p = 0.959), spherical equivalent (0.006 D in the LASIK group vs. 0.004 D in the PRK group, p = 0.173), MTF cutoff value (44.55 in the LASIK group vs. 43.36 in the PRK group, p = 0.438), Strehl ratio (0.231 in t he LASIK group vs. 0.251 in t he PRK group, p = 0.293), or OSI (0.46 in the LASIK group vs. 0.41 in the PRK group, p = 0.470).
Furthermore, three months after surgery, neither group showed significant differences between preoperative and postoperative visual acuity (LASIK, p = 0.255; PRK, p = 0.196) or optical quality (MTF cutoff value, p = 0.659 for LASIK and p = 0.602 for PRK; Strehl ratio, p = 0.114 for LASIK and p = 0.969 for PRK; OSI, p = 0.632 for LASIK and p = 0.300 for PRK).
We drew mean preoperative and postoperative MTF curves (Figs. 8 and 9) as functions of the spatial frequency. These plots show that MTF recovered within one week after LASIK and three months after PRK.
We also made cumulative graphs of UDVA and OSI one month after PRK. Of the patients who noted no visual problems in daily life, 56% had UDVA values greater than 0.8 (logMAR <0.1). However, only 35% patients had OSI values less than 0.5, which was the preoperative average (0.439). These results suggest that optical quality recovers slightly more slowly than UDVA after PRK.
Several studies have reported on clinical analysis of retinal image quality using the double-pass technique. Vilaseca et al. [23] evaluated optical quality after LASIK and reported that the changes depended on the patient's preoperative optical quality. Kamiya et al. [24] assessed the effect of aging on optical quality in a normal population and found that the MTF cutoff value and Strehl ratio decrease and the OSI increases with age. The double-pass technique has been used to evaluate optical quality in contact lens wearers [25,26] and in patients with IOL [27,28].
Ondategui et al. [18] used a d ouble-pass system to compare optical quality after LASIK and PRK for mild-to-moderate myopia. Our results differed from those of Ondategui et al., who found that retinal image quality was significantly reduced to a similar degree after both LASIK and PRK. It seems likely that the differences in these findings resulted from the different surgical instruments used. We used the Wave Eye-Q laser system for ablation, while Ondategui et al. [18] used the MEL 80 excimer laser system (Carl Zeiss Meditec). To prepare the LASIK flap, we used the Visumax femtosecond laser system, while they used the Amadeus microkeratome (Ziemer Group, Port, Switzerland). We also performed each assessment of optical quality twice using the OQAS II and adopted the better results.
In conclusion, the optical quality after laser vision correction recovered to the preoperative level, and laser vision correction is therefore efficacious for correction of myopia. The double-pass system was a useful tool for clinical assessment of optical quality and will be useful for evaluating optical quality after laser vision correction.






 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print






