A Case of Intravitreal Bevacizumab Injection for the Treatment of Choroidal Neovascularization in Angioid Streaks
Article information
Abstract
A 56-year-old Korean woman presented with decreased visual acuity of the right eye. She had a history of two photodynamic therapy treatments for choroidal neovascularization (CNV) due to angioid streaks in her left eye with central scarring and low visual acuity. She was diagnosed with subfoveal CNV due to angioid streaks in her right eye and treated with six intravitreal bevacizumab (1.25 mg / 0.05 mL) injections over one year. Best corrected visual acuity improved from 20 / 125 at baseline to 20 / 50 at the final visit. The area of CNV had changed into a fibrotic scar by the final visit, and fluorescein angiography and indocyanine green angiography revealed no evidence of leakage. Optical coherence tomography showed that central macular thickness decreased from 311 µm at baseline to 203 µm with complete resolution of subretinal and intraretinal fluid at the final visit. Intravitreal bevacizumab for CNV associated with angioid streaks prevented the progression of disease and resulted in the improvement of visual acuity after one year of follow-up in our patient.
Angioid streaks are irregularly radiating gray lines that extend from the area around the optic disc. Angioid streaks result from rupture or dehiscence of a calcified and brittle Bruch's membrane between the retinal pigment epithelium and the choroid. Angioid streaks may be idiopathic, but are associated with systemic diseases in about half of the patients, such as Paget's disease, pseudoxanthoma elasticum, Ehlers-Danlos syndrome or sickle cell anemia [1]. Choroidal neovascularization (CNV) is the major cause of vision loss associated with angioid streaks. CNV occurs in 72% to 86% of eyes with angioid streaks, is often bilateral, and has poor prognosis if left untreated [2-4].
Laser photocoagulation has been widely used to treat juxtafoveal and extrafoveal CNV. However, a high rate of recurrence and laser-induced scar progression toward the fovea has been reported [5,6]. Subfoveal lesions have been treated with photodynamic therapy (PDT) with verteporfin. Published reports of PDT have documented contradictory results. Some authors present short-term benefits of PDT in the treatment of CNV secondary to angioid streaks and suggest that PDT may limit or delay visual damage [7,8]. However, the long-term results of PDT are disappointing and include enlargement of the CNV lesion to a disciform scar and associated visual loss [9-12].
In recent years, an anti-VEGF agent has been widely used as a new treatment for CNV. Intravitreal bevacizumab (Genentech, South San Francisco, CA, USA) has been effective in the treatment of CNV secondary to age-related macular degeneration and pathologic myopia [13,14]. To date, the results of intravitreal bevacizumab for the treatment of CNV due to angioid streaks have been reported in case series with most eyes maintaining or even improving in visual acuity [15-18].
However, most of these reports have no indocyanine green angiography (ICGA) data or are limited to short term follow-up. In this case report, we present the clinical course, including ICGA results, of a patient with subfoveal CNV secondary to angioid streaks treated with intravitreal bevacizumab, who exhibited disease progression despite previous PDT and was followed up for 12 months.
Case Report
A 56-year-old Korean woman presented with blurred vision in the right eye of two months duration. She received a PDT treatment for CNV with angioid streaks in her right eye at another medical center one month before presentation. She complained of deteriorated visual acuity of the right eye after PDT treatment. She also had a history of two PDT treatments for CNV with angioid streaks in her other eye at another medical center four years prior. She was diagnosed with pseudoxanthoma elasticum by skin biopsy at that time.
Ocular examination revealed a best corrected visual acuity (BCVA) of 20 / 125 in the right eye and 20 / 800 in the left eye at the initial visit. Fundus examination revealed peripapillary angioid streaks in both eyes, a grayish subfoveal lesion with mild subretinal exudates in the right eye, and a large disciform scar at the macula in the left eye. Unfortunately, a color fundus photograph from the initial visit was not available. Fluorescein angiography (FAG) and ICGA were performed with a Heidelberg retina angiograph using a scanning laser ophthalmoscope after an intravenous injection of 5 mL of 10% fluorescein sodium (Fluorescite Injection; Alcon, Fort Worth, TX, USA) and 25 mg of indocyanine green (Dong In Dang Pharm., Siheung, Korea) dissolved in 10 mL of sterile water. The last images were obtained at least 30 minutes after the injection of the dye. FAG showed subfoveal classic CNV associated with leakage and peripapillary hyperfluorescence corresponding to the angioid streaks in the right eye. ICGA showed a more distinct margin of subfoveal CNV in early phase than FAG and a peau d'orange appearance in the posterior pole with hyperfluorescent angioid streaks connected to the CNV lesion in late phase, which were not seen in FAG. Both FAG and ICGA of the right eye revealed an increased CNV lesion size and progression to the center of the fovea despite the previous PDT treatment that was performed at another medical center. Optical coherence tomography (OCT) was performed using OCT 3 (Carl Zeiss Meditech, Dublin, CA, USA), and a central macular thickness (CMT) was obtained using a fast macular map protocol. OCT scans of the right eye revealed a hyperreflective subfoveal choroidal neovascular membrane with cystoid macular edema and neurosensory serous detachment. CMT was 311 µm in the right eye (Fig. 1).

Early (A) and late (B) phase of fluorescein angiography (FAG) showing previous juxtafoveal classic choroidal neovascularization (CNV) that increased and progressed into the subfoveal area despite a photodynamic therapy treatment. (C) Early phase of indocyanine green angiography showing a more distinct margin of the subfoveal CNV lesion than FAG. (D) Late phase of indocyanine green angiography showing a peau d'orange appearance in the posterior pole with hyperfluorescent angioid streaks connected to the CNV lesion in late phase, which were not seen in FAG. (E) Optical coherence tomography showing a hyperreflective subfoveal choroidal neovascular membrane with cystoid macular edema and neurosensory serous detachment.
Follow-up visits were carried out one week after intravitreal bevacizumab injection and then monthly for 12 months. For each visit, the BCVA using a Snellen chart, intraocular pressure and any complications were assessed. FAG, ICGA and OCT were performed one month after each injection to evaluate the effect of the intravitreal bevacizumab injection. Additional treatment was administered when the lesion exhibited persistent leakage or growth on FAG and ICGA and when the presence of subretinal or intraretinal fluid on OCT combined with decreasing visual acuity was detected.
After four consecutive monthly intravitreal injections of bevacizumab (1.25 mg / 0.05 mL) in the right eye, BCVA improved from 20 / 125 at baseline to 20 / 50 at four months. A color fundus photograph at this time indicated resolution of subretinal exudates and a contracted subfoveal lesion in the right eye. FAG and ICGA revealed a minimal amount of persistent leakage at one, two and three months, although CNV size and leakage decreased markedly. Both FAG and ICGA indicated that there was no leakage of CNV and the greatest linear diameter of the lesion decreased from 1,280 µm at baseline to 730 µm at 4 months. However, ICGA displayed a more distinct margin of CNV than FAG despite the presence of diffuse pigment migration at the fovea. OCT showed that CMT decreased from 311 µm at baseline to 210 µm and was absent of subretinal fluid at 4 months. Nevertheless, complete resolution of intraretinal fluid on OCT did not occur by 4 months.
BCVA decreased from 20 / 50 at 4 months to 20 / 63 at 8 months. A color fundus photograph exposed a newly developed subretinal hemorrhage and exudates at 8 months. FAG and ICGA revealed that a new CNV lesion developed at the superior margin of the previous lesion at 8 months. CMT increased from 210 µm at 4 months to 233 µm at 8 months.
Therefore, two additional, consecutive, monthly intravitreal bevacizumab injections were required. After a total of six intravitreal bevacizumab injections, BCVA improved from 20 / 125 at baseline to 20 / 50 at the final visit. A color fundus photograph showed that the CNV area had changed into a contracted fibrotic scar with complete resolution of subretinal hemorrhage and exudates at the final visit. FAG and ICGA revealed no angiographic evidence of leakage. OCT demonstrated CMT decreased from 311 µm at baseline to 203 µm with complete resolution of intraretinal fluid at the final visit (Fig. 2). No injection-related complications or drug-related side effects were observed.
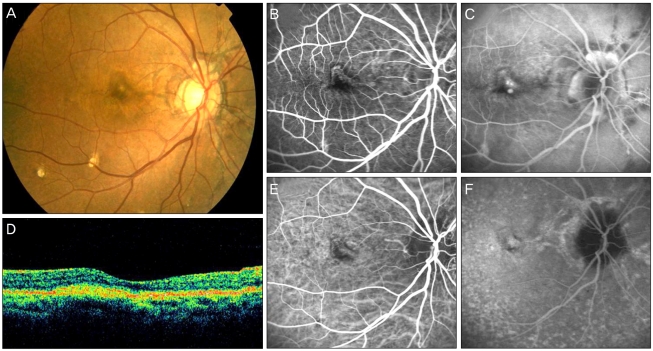
At 12 months after a total of six intravitreal bevacizumab injections. (A) Color fundus photograph showing resolution of subretinal hemorrhage and exudates and the contracted subfoveal lesion. Early (B) and late (C) phase of fluorescein angiography and early (E) and late (F) phase of indocyanine green angiography revealing leakage resolution. (D) Optical coherence tomography showing a decrease in central macular thickness and absence of intraretinal fluid with normal foveal contour.
Discussion
In the present study, PDT was performed for CNV due to angioid streaks in the right eye of the patient at another medical center one month before presentation. However, visual acuity deteriorated after PDT, and juxtafoveal CNV progressed to the subfoveal area with lesion enlargement. In addition, her left eye revealed disciform scarring with low visual acuity despite two PDT treatments. These findings correspond to earlier results that reported disease progression with a decrease in visual acuity after PDT for CNV in angioid streaks [9-12]. However, visual acuity improved with no angiographic evidence of leakage and a decrease in CMT at four months after four consecutive monthly intravitreal bevacizumab injections. These findings correspond with earlier studies reporting that intravitreal bevacizumab stabilized or improved visual acuity with favorable anatomic outcomes in either naïve eyes or eyes that had failed previous PDT treatment [15,16].
A new CNV lesion was noted at the superior margin of the previous CNV area at eight months (four months after the last intravitreal bevacizumab injection) in the present study. Fortunately, visual acuity increased with no leakage on angiography or flattening of retinal edema on OCT after two additional consecutive monthly intravitreal bevacizumab injections.
These results are consistent with long term follow-up studies that reported that the mean interval between retreatments was about four months and intravitreal bevacizumab injections had to be repeated in all patients [17,18].
In a retrospective study of nine eyes in six patients, Wiegand et al. [17] reported that visual acuity stabilized or improved in eight eyes (88.8%) with a reduction in retinal thickness in all eyes after a mean follow-up of 19 months. In a prospective study with eleven patients, Neri et al. [18] reported that visual acuity stabilized or improved with reduced or stable CNV size in all eyes at 20 months. These long term follow-up results suggest that early retreatment may ensure favorable functional and anatomical outcomes and prevent disease progression.
Anatomical improvement was associated with a concomitant increase in visual acuity in the present study. Our result are consistent with previous studies reporting improvement of functional results correlated with a decrease in the greatest lesion height on OCT [15,16]. In addition, the visual acuity deterioration was followed by an increase of CMT in the present study. Therefore, regular follow-up with visual acuity testing and close observation of the macula using OCT may inform decisions for early intervention in order to prevent disease progression.
In contrast to previous therapeutic regimens, such as laser photocoagulation and PDT, that often result in disciform scarring and irreversible loss of function of the retinal pigment epithelium (RPE) and overlying retina [10], intravitreal bevacizumab injection in the present study resulted in improvement of visual and anatomic outcomes without scar formation. Intravitreal bevacizumab injection may have antiexudative and antiproliferative effects while preserving the RPE and overlying retina [15,19].
The results obtained from our patient indicate that intravitreal bevacizumab for CNV associated with angioid streaks may prevent the progression of disease and result in the improvement of visual acuity.
Notes
No potential conflict of interest relevant to this article was reported.