Treatment of Branch Retinal Artery Occlusion With Transluminal Nd:YAG Laser Embolysis
Article information
Abstract
The purpose of this paper was to report a successful treatment of transluminal Nd:YAG laser embolysis (NYE) for branch retinal artery occlusion (BRAO) with visible emboli. Two patients with acute, severe vision loss secondary to a branch retinal artery occlusion with visible emboli in one eye underwent NYE. A complete ocular examination was performed which included biomicroscopy of the posterior pole of the retina, intraocular pressure measurement, fundus color photographs, and fluorescein angiography (FA). After the NYE, the two patients showed dramatic improvements in best-corrected visual acuity, as well as, immediate and dramatic restorations in flow past the obstructed arteriole in FA. NYE is a treatment modality to be considered in patients with BRAO who present acutely with severe vision loss and a visible embolus.
Branch retinal artery obstruction (BRAO) accounts for 38% of acute retinal arterial obstructions.1 BRAO usually results from emboli, although non- embolic causes such as vasculitides, coagulopathies, and vasospasms resulting from migraines and inflammatory conditions do occur. Emboli are visible on funduscopic examination in 62% of cases. Risk factors for BRAO development include hypertension, carotid occlusive disease or atherosclerosis, coronary artery disease, and hypercholesterolemia. Branch retinal artery obstructions typically occur at vessel bifurcations, and 98% of cases involve the temporal vessels.2 There is no established effective treatment for BRAO.
Recent studies indicated that Nd:YAG laser embolysis (NYE) treatment resulted in successful restoration of retinal blood flow and improved best-corrected visual acuity (BCVA).3,4 The present report describes outcomes following the treatment of two cases of BRAO with NYE.
Case Reports
Case 1
A 68-year-old woman presented with decreased visual acuity (VA), and 20 hours earlier had noticed a visual field defect in the superior half of her right eye. Her medical history was unremarkable except for a history of hyperlipidemia. BCVA was 20/63 at the initial examination. Slit lamp biomicroscopy and fundus examination revealed intraretinal edema with inferior retinal whitening in addition to a visible Hollerenhorst plaque. Fluorescein angiography (FA) revealed an arterial filling defect along the inferotemporal arcade, distal to the corresponding embolus with foveal ischemia (Fig. 1).
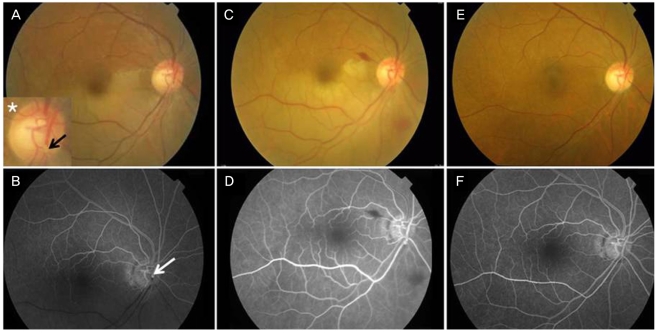
Color fundus photographs and fluorescein angiography (FA) showing branch retinal artery obstruction in case 1. (A) Color fundus photograph demonstrating an intraluminal embolus (arrow) and whitening of the retina along the inferior and temporal vascular arcades. inserted: the asterisk panel '*' shows a magnification of the embolus. (B) FA of the same patient showing obstructed blood flow at the site of the embolus and a downstream filling defect. (C) Color fundus photograph of the same patient taken five days after Nd:YAG laser embolysis (NYE). Note the small amount of vitreous hemorrhage around the disc. (D) Fluorescein angiography (FA) of the same patient five days after NYE showing perfusion at the site of the embolus and restoration of the downstream blood flow. (E) Color fundus photograph taken three months after NYE. There was no remaining vitreous hemorrhage. (F) FA at three months after NYE showing a patent retinal artery with good blood flow and no neovascularization.
The initial treatment involved anterior chamber paracentesis, use of an IOP-lowering agent, and ocular massage. Approximately 12 hours later, BCVA of her right eye decreased to 20/200. A Goldmann three mirror lens was used to focus an Nd:YAG laser onto the arterial embolus. The laser energy level commenced at 0.5 mJ and was increased to 1 mJ (about 12 pulses) until the embolus was partially or completely shattered. After shattering the embolus, a small amount of vitreous hemorrhage was noted inferior to the optic disc. Five days after treatment, FA showed no evidence of the emboli, and retinal arteriolar blood flow had been restored. BCVA improved to 20/80. At two months after NYE, BCVA was 20/25 with no remaining vitreous hemorrhage. At three months after NYE, BCVA was 20/20 and FA showed that the branch retinal artery and all arterioles were patent with good flow. At ten months after NYE, BCVA remained at 20/20, and there were no other complications.
Case 2
An 82-year-old woman presented with a four-day history of progressive decrease in VA in her left eye. Her medical history was unremarkable. At presentation, BCVA was 20/200, which was lower than the reading of 20/32 taken six months earlier. Slit-lamp biomicroscopy revealed a large plaque in the associated branch retinal artery on the disc of the left eye. FA showed an arterial filling defect along the superotemporal arcade distal to the corresponding embolus (Fig. 2). A macular contact lens was used to deliver the Nd:YAG laser to the plaque. Pulsing commenced with one pulse at 0.5 mJ, and the energy was increased to 1 mJ, at which a total of eight pulses were applied to the plaque. A small amount of vitreous hemorrhage over the arteriole was noted which resulted in cessation of the laser treatment despite the remaining embolus. The following day, vitreous hemorrhage decreased slightly and laser treatment was recommenced (1 mJ×ten pulses). The large embolus was ruptured, and recirculation around the macula was noted. However, a partial embolus fragment remained in the associated arteriole. On the second day after NYE, BCVA had improved to 20/100, and the vitreous hemorrhage remained present. On the third day after NYE, FA showed restoration of the retinal arteriolar blood flow. Forty days after NYE, BCVA had improved to 20/32. At four months after NYE, FA showed no retinal neovascularizations, and BCVA remained at 20/32.
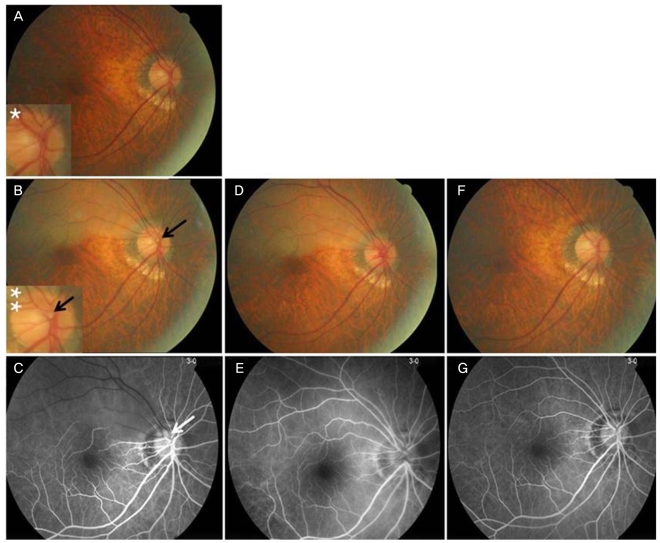
Color fundus photographs and fluorescein angiography showing branch retinal artery obstruction (BRAO) in Case 2. (A) Color fundus photograph six mon prior to BRAO. The asterisk panel '*' shows a magnification of the disc and indicates no transluminal embolus. (B) Color fundus photograph showing a superior temporal branch retinal artery occlusion. Note the transluminal embolus (arrow) and opacification of the retina along the superior and temporal vascular arcades. The double asterisk panel '**' shows a magnification of the transluminal embolus. (C) Fluorescein angiography (FA) showing the filling defect in the arteriole corresponding to the intraluminal embolus. (D) Color fundus photograph taken three days after Nd:YAG laser embolysis (NYE). Note the small amount of vitreous hemorrhage around the disc. (E) FA three days after NYE showing restoration of retinal blood flow. (F) Color fundus photograph taken two mon after NYE. Note the spontaneous clearing of the small vitreous hemorrhage. (G) FA two mon after NYE showing a return of retinal blood flow.
Discussion
Recent reports showed immediate restoration of retinal blood flow after NYE, in addition to rapid restoration of BCVA. However, complications such as vitreous hemorrhage and subretinal hemorrhage were observed.3,4 In the present cases, laser treatment resulted in dramatic improvement in BCVA and restoration of retinal blood flow despite a small amount of vitreous hemorrhage.
Mason et al.5 reported that visual prognosis after BRAO appeared to correlate with presenting VA, and that eyes with an initial VA of 20/40 or better usually remained at 20/40 or better. Individuals with poor VA (e.g., 20/100 or worse) generally did not show significant improvement. They concluded that it may be misleading to indicate that 80% of eyes with BRAO improve to 20/40 or better (as described in previous reports) when final BCVA is so closely related to presenting BCVA.
In conclusion, the presenting VA may be essential in deciding whether to pursue aggressive treatment. Therefore, NYE should be considered an effective treatment in patients with BRAO with visible emboli.