Intermittent exotropia has been categorized into the following types: basic, divergence excess, pseudodivergence excess, and convergence insufficiency. The pseudodivergence excess type has been subclassified into tenacious proximal fusion (TPF) and high accommodative convergence/accommodation ratio (AC/A) types [
1]. Patients with an initial distance deviation that exceeds the near deviation by 10 prism diopters (PD), but with a near deviation angle similar to the distance deviation angle after 1 hour of monocular occlusion have been defined as having TPF [
2]. TPF has been reported to occur in patients who have a slow-to-dissipate fusional vergence that can be suspended with prolonged occlusion [
2]. Patients with high AC/A type can be identified by an increase in near deviation measured through +2.50 diopters (D) or +3.00 D spherical lenses [
3,
4]. This subclassification is complicated; however, several studies have reported that the prognosis of patients differed between the two types. Specifically, patients with TPF show good surgical outcomes, whereas patients with high AC/A type have poorer results, with most experiencing consecutive esotropia after lateral rectus recession [
1,
5,
6].
To our knowledge, no previous studies have directly compared the features and surgical outcomes of patients with TPF and high AC/A types of intermittent exotropia. This study compared groups of these patients.
Materials and Methods
This study retrospectively analyzed all patients with TPF or high AC/A intermittent exotropia who underwent bilateral lateral rectus recession between January 2011 and January 2017 and were followed up for more than 12 months. Patients with a distance deviation angle exceeding the near deviation angle by more than 10 PD, but who experienced a reduction in the difference between distance and near deviation angles to less than 10 PD after monocular occlusion for 1 hour were classified with TPF type intermittent exotropia. High AC/A ratio type was defined as an exodeviation in which the near exodeviation increased to within 10 PD of the distance exodeviation after prolonged monocular occlusion and the use of +3.00 D sph lenses at near. High AC/A ratios greater than 7 : 1 were confirmed by the lens gradient method [
7]. The present study was approved by the institutional review board of Haeundae Paik Hospital (HPIRB 2017-07-620-001), and adhered to the tenets of the Declaration of Helsinki. Informed consent was waived due to the retrospective nature of the study.
Patients with other types of strabismus, including paralytic or restrictive strabismus; amblyopia or other ocular disease; a history of ocular surgery, including prior strabismus surgery; nystagmus; congenital anomaly; neurologic abnormality; or chromosomal or systemic disease were excluded. Visual acuity was measured after correction of refractive error. Preoperative stereopsis was evaluated using Titmus stereo tests (Stereo Optical, Chicago, IL, USA), and binocular function was evaluated using Worth's 4-dot tests (flashlight type; Mag Instrument, Ontario, CA, USA), with the latter performed at near (33 cm) and distance (6 m) while wearing red/green glasses in a dark room. Worth's 4-dot tests were designed to display 4 apertures approximately 6 mm in diameter, with all dots spaced equidistantly on a 34 mm diameter circle. The 4 dots transmitted red light at the 12 o'clock position, green light at the 3 and 9 o'clock positions, and white light at the 6 o'clock position; interpretable responses were fusion, suppression, and diplopia.
After the cover-uncover test, an alternate prism cover test was performed using an accommodative target at 33 cm near and 6 m distance. The near deviation angle was measured again in all patients after monocular occlusion for 1 hour. Subsequently, a +3.00 D spherical lens was placed in front of the eye, and the deviation angle at near was measured while blocking fusional convergence. All surgeries were performed under general anesthesia by one of the authors (SJL). The surgical dose of bilateral lateral rectus recession was determined by Park's method based on distance and large near deviation angles following monocular occlusion tests in patients with TPF and with +3.00 D spherical lens tests in patients with high AC/A ratio, which were the largest deviation angles before the surgery. Deviation angles were measured on postoperative day 1 and after 1 and 12 months. Positive values indicated exodeviation, and negative values indicated esodeviation. Surgical success was defined as distance and near deviation angles <±10 PD after 12 months and no complaints of diplopia. Recurrence was defined as exotropia ≥10 PD at distance or near, and consecutive esotropia was defined as esotropia ≥10 PD at distance or near. All statistical analyses were performed using PASW Statistics ver. 18.0 (SPSS Inc., Chicago, IL, USA). Comparisons were determined by the chi-square test, Mann Whitney U-test, and Pearson correlation, as appropriate. A p-value <0.05 was considered statistically significant.
Results
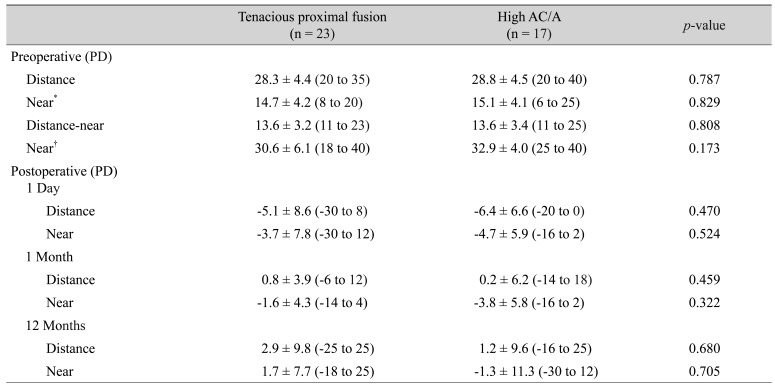
Twenty-three patients, consisting of 11 male and 12 female, were classified as TPF type intermittent exotropia, and 17 patients, 6 male and 11 female, were classified as high AC/A type. Mean age at surgery of TPF and high AC/A types were different (
p = 0.027); however, gender distribution, preoperative corrected visual acuity, follow-up period, mean Titmus stereoacuities, and number of patients with stereoacuities ≤100 sec arc (
Table 1) were not statistically significantly different between the two groups.
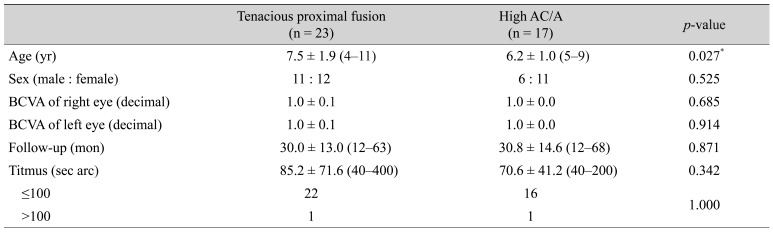
Worth's 4-dot tests at distance showed no significant differences in the proportion of patients with fusion, suppression, and diplopia responses between the groups (
Table 2). At near, the proportion of patients with diplopia was significantly higher in the high AC/A group than in the TPF group (
p = 0.029). The proportions of patients with fusion and suppression were higher in the TPF group, but these differences were not statistically significant.
There were no significant differences in angle of deviation preoperatively or at 12 months postoperatively between patients with and without diplopia responses at near on the Worth 4-dot test in both groups (TPF group, p = 0.147 and 0.129; high AC/A group, p = 0.239 and 0.210). In addition, there was no significant relationship between surgical success rate and diplopia response at near on the Worth 4-dot test in both groups (TPF group, p = 0.261; high AC/A group, p = 0.600).
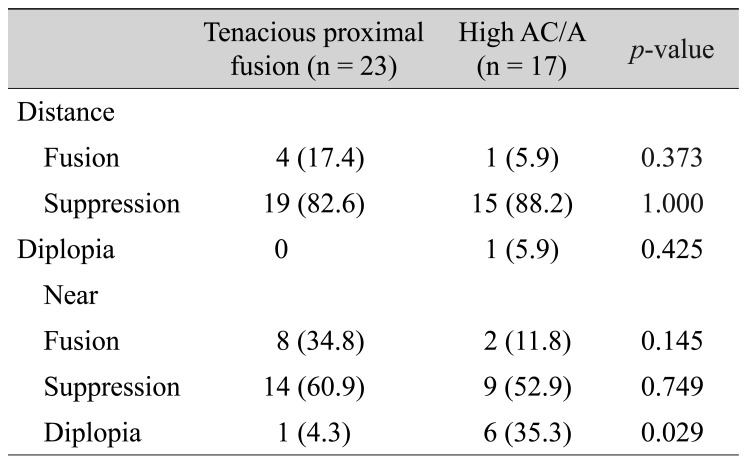
Mean preoperative deviation angles of patients with TPF type and high AC/A type intermittent exotropia were 28.3 ± 4.4 and 28.8±4.5 PD, respectively, at distance (
p = 0.787) and 14.7 ± 4.2 and 15.1 ± 4.1 PD at near before monocular occlusion tests or before +3.00 D spherical lens tests (
p = 0.829). Differences of distance-near deviation angle were 13.6 ± 3.2 and 13.6 ± 3.4 PD in the TPF and high AC/A groups, respectively (
p = 0.808) (
Table 3). Mean preoperative deviation angle at near was 30.6 ± 6.1 PD after monocular occlusion tests in the TPF group and 32.9 ± 4.0 PD after +3.00 D spherical lens tests in the high AC/A group (
p = 0.173). At 12 months after surgery, the mean deviation angles in the TPF and high AC/A groups were 2.9 ± 9.8 and 1.2 ± 9.6 PD, respectively, at distance (
p = 0.680) and 1.7 ± 7.7 and −1.3 ± 11.3 PD at near (
p = 0.705).
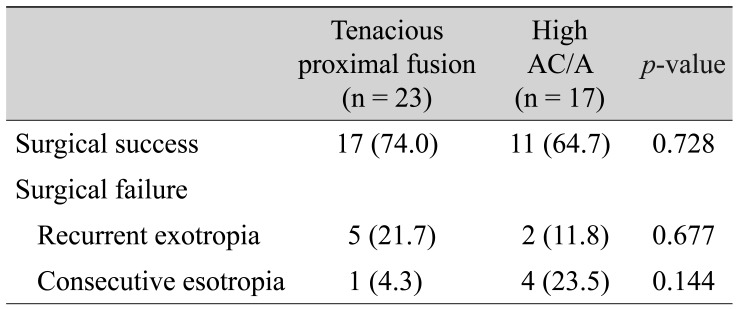
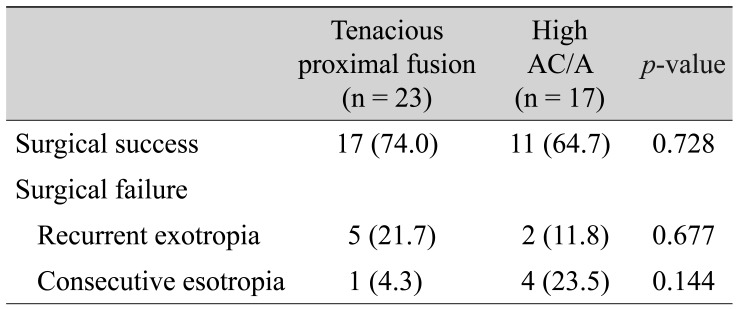
Surgical success after 12 months was observed in 17 (74.0%) of 23 patients with TPF and 11 (64.7%) of 17 patients with high AC/A intermittent exotropia (
p = 0.728) (
Table 4). Five patients in the TPF group and 2 in the high AC/A group experienced recurrence (
p = 0.677), with 1 and 4, respectively, experiencing consecutive esotropia (
p = 0.144). Of the patients who experienced recurrence, 4 in the TPF group and 1 in the high AC/A group changed to basic type intermittent exotropia, and the rest were unchanged.
Discussion
Pseudodivergence excess has been subclassified into TPF and high AC/A ratio types [
1]. A smaller near deviation angle may be due to greater fusional stimulus to near target or to accommodative convergence by a larger and brighter image on the retina, which results from a closer target [
8]. Prolonged monocular occlusion and use of plus spherical lenses at near have been found to affect different convergence mechanisms [
9], with monocular occlusion suspending fusional convergence (TPF type) and plus spherical lenses relaxing accommodative convergence (high AC/A ratio type). A comparison of binocular function in patients with basic and pseudodivergence excess types of intermittent exotropia found that all patients with pseudodivergence excess type showed fusion responses on Worth's 4-dot tests at near [
10].
In our study, the binocular function of patients with TPF and high AC/A types, as evaluated by Worth's 4-dot test, did not differ at distance. However, the proportion of patients with diplopia at near was significantly higher in patients with high AC/A type than in those with TPF type intermittent exotropia. Only objects that formed in the fovea of the fixating eye form on non-corresponding retinal points at a small deviation angle. Peripheral objects form on the corresponding retinal points and are located in Panum's fusional area. Thus, peripheral fusion can exist even in the absence of central fusion, and interruption in this peripheral fusion may result in a diplopia response.
Light is a poor accommodative target because fine detail is not required and accommodation is not necessary to see the light [
11]. In this study, a high rate of diplopia was thought to be caused by an increase in near deviation angle resulting from reduction in accommodative convergence when measuring binocular function at near while looking at the light from the Worth's 4-dot tests in the high AC/A group. Therefore, additional studies to better understand this hypothesis are needed.
Postoperative measurements of mean deviation angle over time showed that distance had a larger value in the direction of exodeviation than near in both TPF and high AC/A intermittent exotropia. In both types, however, the distance deviation angle was larger than the near deviation angle in the direction of esodeviation at 1 day. This could be attributable to temporary reductions in fusional and accommodative convergence immediately after surgery.
Unilateral medial rectus resection and lateral rectus recession have been recommended for patients with pseudodivergence excess type of intermittent exotropia [
2,
12]. However, bilateral lateral rectus recession was also found to be effective in treating pseudodivergence excess type exotropia by correcting both the near and distance deviation angles [
13]. Surgical success rates have been reported to be similar in patients who undergo unilateral medial rectus resection and lateral rectus recession or bilateral lateral rectus recession for pseudodivergence excess type exotropia [
14]. In our study, as previously reported, the mean near deviation angle in patients with high AC/A type intermittent exotropia showed esotropia after 12 months; however, this esotropia was not meaningful compared with that in the TPF type. Although there were no significant differences in surgical success rate or incidence of consecutive esotropia between patients with TPF or high AC/A type, the success rate of the high AC/A type was 10% lower than that of the TFT type, and the high AC/A type was more likely to develop consecutive esotropia than the TFT type.
Limitations of this study include small sample of the patients and its retrospective design. Furthermore, only Worth's 4-dot test was performed preoperatively to evaluate binocular function.
In conclusion, the rate of diplopia response on Worth's 4-dot tests at near was higher for patients with high AC/A type than those with TPF intermittent exotropia. However, there was no significant difference in surgical success rate following bilateral lateral rectus recession or in the incidence of consecutive esotropia.
Notes
This study was presented as poster at the 118th annual meeting of the Korean ophthalmological Society in Busan, Korea, November 3-5, 2017.
Notes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
REFERENCES
1. Kushner BJ, Morton GV. Distance/near differences in intermittent exotropia.
Arch Ophthalmol 1998;116:478-486.


2. Burian HM. Exodeviations: their classification, diagnosis and treatment.
Am J Ophthalmol 1966;62:1161-1166.


3. Brown H. Exodeviations: their classification, diagnosis, and treatment. In: Haik GM, Strabismus Symposium of the New Orleans Academy of Ophthalmology. St Louis: CV Mosby; 1962. p. 238.
4. Brown HW. Accommodative convergence in exodeviation.
Int Ophthalmol Clin 1971;11:39-45.


5. Edelman PM, Brown MH, Murphree AL, Wright KW. Consecutive esodeviation, then what?
Am Orthopt J 1988;38:111-116.

6. Raab EL, Parks MM. Recession of the lateral recti: early and late postoperative alignments.
Arch Ophthalmol 1969;82:203-208.


7. Scheiman M, Wick B. Clinical management of binocular vision. Philadelphia: Lippincott Williams & Wilkins; 2008. p. 282-317.
8. Scobee RG. The oculorotary muscles. 2nd ed. St Louis: Mosby-Year Book; 1952. p. 85-90.
9. Helveston EM. The use and abuse of +3.00 D lenses.
J Pediatr Ophthalmol Strabismus 1974;11:175-176.

10. Lee SY, Kim HY, Lee YC. The comparison of binocular function of basic and simulated divergence excess type in intermittent exotropia.
J Korean Ophthalmol Soc 2005;46:682-687.

11. Wright KW, Strube YN. Pediatric ophthalmology and strabismus. 3rd ed. New York: Oxford University Press; 2012. p. 265-280.
12. Burian HM, Spivey BE. The surgical management of exodeviations.
Trans Am Ophthalmol Soc 1964;62:276-306.


13. Kushner BJ. Exotropic deviations: a functional classification and approach to treatment.
Am Orthoptic J 1988;38:81-93.

14. Lee SY, Sim JH, Lee YC. Comparison of surgical results according to surgical methods in simulated divergence excess exotropia. J Korean Ophthalmol Soc 2004;45:614-619.
Table 1
Basic characteristics of patients with intermittent exotropia
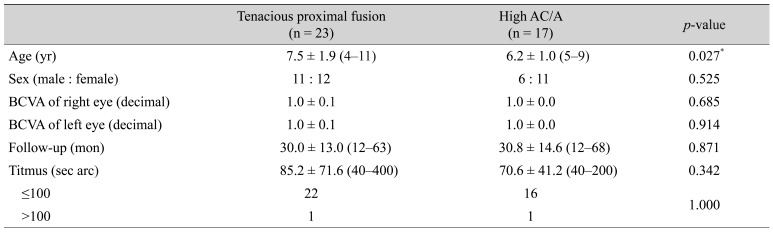
Table 2
Patient responses on the Worth 4-dot test at distance and at near
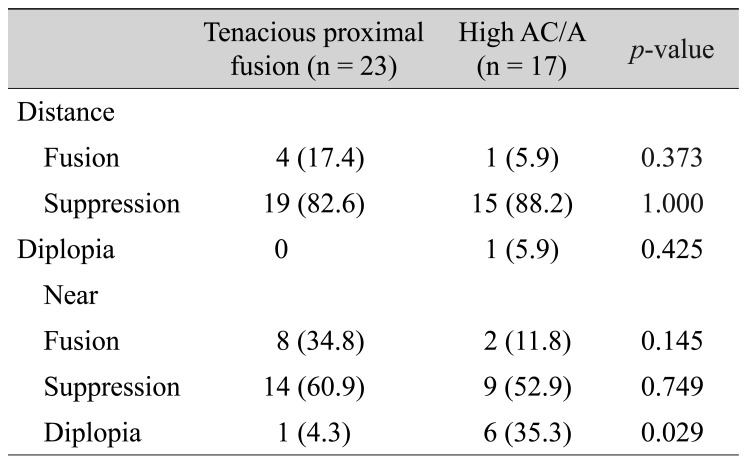
Table 3
Preoperative and postoperative mean angles of deviation in patients with tenacious proximal fusion or high AC/A intermittent exotropia
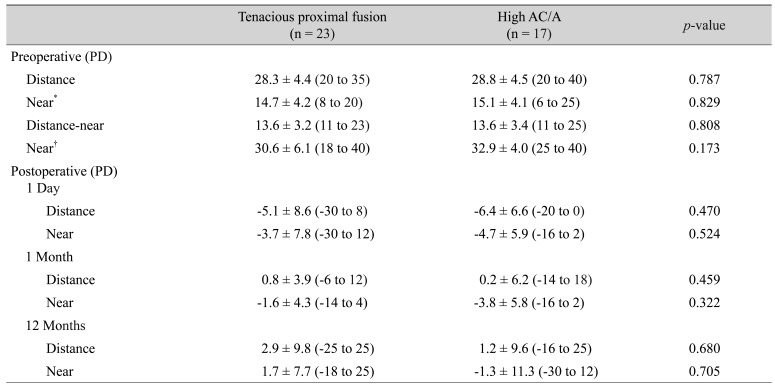
Table 4
Surgical outcomes after 12 months






 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print



