Dear Editor,
Cytomegalovirus (CMV) retinitis is an opportunistic infection that usually affects immunocompromised patients. Severe intraocular CMV infections in immunocompromised patients are typically asymptomatic, and can involve mild anterior uveitis [1]. One recent paper reported retinal arterial occlusion due to CMV infection in elderly people [1]. To the best of our knowledge, we report the first case of ocular ischemic syndrome (OIS) that initially presented as CMV retinitis.
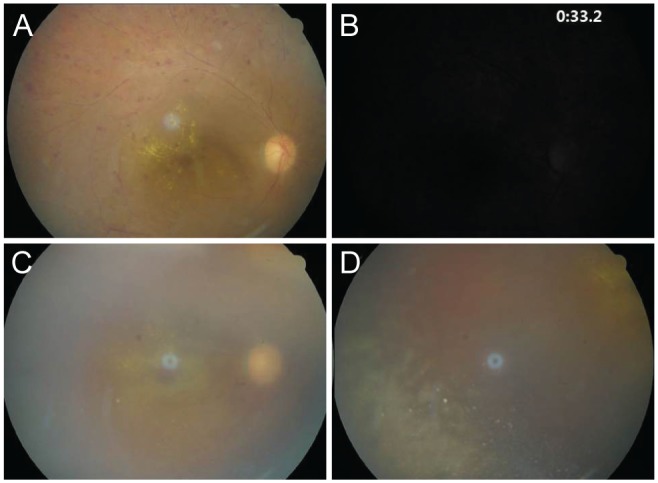
A 71-year-old man with diabetes presented with a oneweek history of blurred vision in the right eye. The patient had a history of lymphoma, which was in complete remission for 2 years. In the right eye, the patient could count fingers at 50 cm with a relative afferent pupillary defect. The intraocular pressure was 12 mmHg. Examination of the anterior segment was normal. Fundus examination of the right eye demonstrated 1+ vitreous cells, a whitish edematous retina, retinal hemorrhage with exudate, and narrowing and segmentation of the retinal arteries (Fig. 1A). Subsequent fluorescein angiography showed delayed choroidal and arteriolar filling, suggestive of OIS (Fig. 1B). We performed brain and neck magnetic resonance angiography, which were normal. There was no evidence of recurrent lymphoma. The patient was observed without additional treatment such as intravitreal steroid injection or panretinal photocoagulation. One month later, the patient complained of worsening visual acuity in the right eye. The right-sided vision included only light perception. The intraocular pressure increased to 30 mmHg. Slit lamp examination demonstrated 3+ cells in the anterior chamber and iris neovascularization. Fundoscopy revealed dense vitritis with dense retinal whitening in the inferotemporal area, suggestive of infectious retinitis (Fig. 1C, 1D). Blood tests were unrevealing of any immune dysfunction. The complete blood count was normal. Serologic tests for human immunodeficiency virus, varicella zoster virus and herpes simplex virus were negative. An anterior chamber paracentesis was performed for polymerase chain reaction. The polymerase chain reaction results were positive for CMV, and negative for varicella-zoster virus, herpes simplex virus, and Epstein-Barr virus.
An intravitreal injection of ganciclovir was administered. The patient was also treated with oral valganciclovir. The retinitis and vitritis improved gradually over the following week; however, the retinal vessels appeared slightly attenuated. Two months later, surgery for neovascular glaucoma was recommended. However, the patient refused further therapeutic interventions given poor visual prognosis and financial concerns.
In immunocompromised patients, CMV retinitis typically causes cotton wool spots along the retinal vessels, accompanied by many retinal hemorrhages [1]. In contrast, CMV infection of the eye in immunocompetent patients is atypical, and usually limited to the anterior segment [2].
Our patient was susceptible to CMV infection given his age and history of diabetes. The immune system function deteriorates with age, leading to profound remodeling and overall decline. These changes increase one's susceptibility to acute viral and bacterial infections [3,4]. Diabetes can also contribute to impaired organ function. Diabetic retinopathy, for instance, is frequently related to the breakdown of the blood-retinal barrier. CMV reaches the retina hematogenously after it first infects the vascular endothelium. Breakdown of the blood-retinal barrier may facilitate subsequent viral spread to the surrounding glial and neuronal cells. The retinal pigment epithelium can eventually become infected. Recently, CMV infection has been reported in association with retinal vessel occlusion [2]. Davis et al. [2] reported that central retinal artery occlusion or large retinal vessel occlusions, although rare, can occur in CMV retinitis. This phenomenon can also spread to the entire retina. To our knowledge, OIS has never been reported as an initial feature of CMV retinitis. OIS is usually reported in association with high-grade stenosis or occlusion of the carotid artery. However, our patient had no signs of carotid stenosis. Therefore, CMV infection may have been the causative factor of extensive large vascular ischemia in this case. This case was puzzling given the patient's immunocompetent state, and clinical features that were atypical for opportunistic CMV infections. This unusual manifestation of OIS and CMV retinitis should increase clinicians' knowledge of the early deficits of CMV retinitis in elderly immunocompetent patients.



 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print






