Dear Editor,
A ventriculoperitoneal (VP) shunt is effective for hydrocephalus. However, the shunt may malfunction due to obstruction, breakage, migration, or infection [1]. Slit ventricle syndrome (SVS) is a rare symptomatic condition presenting with neuroimaging findings of small ventricles in a patient with a VP shunt. Accurate diagnosis can be difficult and adequate treatment may be delayed because neuroimaging of small ventricles can be misinterpreted as a properly working shunt [1,2,3]. In Korea, there have been no reports of SVS presenting with only visual symptoms. We report the case of a pediatric patient with SVS who presented with visual, but not systemic symptoms.
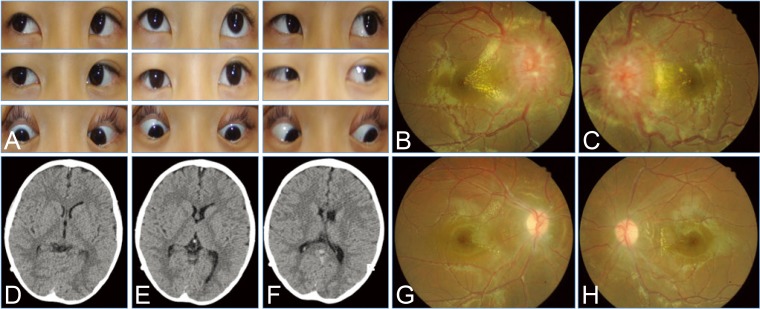
A 10-year-boy visited our ophthalmic department. He was born at 33 weeks of gestation, with a birth weight of 2,030 g. He underwent VP shunt placement at the age of 6 months for hydrocephalus due to intraventricular hemorrhage. During the present visit, he described gradual onset of bilateral visual disturbances and horizontal intermittent diplopia for 1 week. He did not report other systemic symptoms suggesting increased intracranial pressure, such as headache, nausea, vomiting, or altered consciousness level. Visual acuity was 20 / 50 in the right eye and 20 / 20 in the left, but color vision test using an Ishihara plate was decreased in the both eyes. Pupils showed normal response to light and near stimulation. He demonstrated 20 prism diopters esotropia in the right eye, with mild abduction limitation (Fig. 1A). Fundus examination showed optic disc swelling, increased vessel tortuosity, and bilateral macular exudates (Fig. 1B and 1C). Computerized tomography of the brain did not show ventricuolmegaly or other signs of increased intracranial pressure (Fig. 1D-1F). A serologic work-up was conducted to rule out other inflammatory or infectious causes; the results were within normal limits except for a white blood cell count of 12,090/┬ĄL (normal, 4,000 to 10,000). Two weeks later, follow-up computerized tomography was performed instead of intracranial pressure measurement; there was no clear difference compared to previous studies. However, fundus examination revealed more severe optic disc swelling compared to that observed at the previous visit. Shunt revision was performed and visual symptoms gradually improved. Six months later, visual acuity had improved to 20 / 20 in both eyes, and fundus showed no optic disc swelling (Fig. 1G and 1H). He was orthotropic and had no diplopia.
SVS refers to the occurrence of headache, vomiting, and possibly some degree of impaired consciousness and visual deterioration in children with hydrocephalus and VP shunts [3]. The pathogenesis remains unclear. Overdrainage, periodic shunt malfunction, intracranial hypertension, and decreased brain parenchyma compliance to variations in cerebrospinal fluid volume have been proposed as SVS mechanisms. Recent research suggested that lack of ventricular dilation is related to a reduction in brain compliance, analogous to that seen in idiopathic intracranial hypertension [4]. Therefore, diagnosis of SVS can be delayed if systemic symptoms of increased intracranial pressure are absent and neuroimaging findings are negative. As in this case, visual symptoms may be the only clue to shunt malfunction. The anterior and posterior visual pathways and the ocular motor nerves, especially the abducens, are vulnerable to increased intracranial pressure because of their subarachnoid course [2]. Although papilledema is not a sensitive sign of shunt dysfunction in children, it remains a pivotal finding that may suggest shunt dysfunction [5]. Nguyen et al. [2] reported ophthalmic complications of SVS in children, and two of six patients in their study developed optic atrophy later in the disease course. As elevated intracranial pressure related to SVS can lead to permanent visual loss, visual symptoms should not be overlooked in VP shunt patients. In conclusion, SVS can present with visual symptoms occurring in the absence of other neurologic symptoms in pediatric patient. Development of visual symptoms in patients with VP shunts necessitates close follow-up and neurologic work-up to evaluate intracranial pressure.



 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print






