 |
 |
| Korean J Ophthalmol > Volume 32(2); 2018 > Article |
Abstract
Purpose
We evaluated the long-term surgical outcome and lens complications in children with persistent pupillary membrane following removal using vitreous scissors.
Methods
Patients diagnosed with persistent pupillary membrane who received surgical treatment from 1987 to 2012 were retrospectively reviewed. The removal was performed using vitreous scissors after instillation of miotics. The minimum follow-up period after surgery was four years. Factors of age, sex, visual acuity, refractive errors, and complications during or after surgery were evaluated.
Results
A total of 32 eyes of 26 patients were included. The mean age at the initial visit was 22.6 ± 34.7 (range, 0.9 to 141.2) months, and the mean age at surgery was 43.7 ± 36.0 (range, 1.0 to 142.5) months. There were no intraoperative complications using vitreous scissors, and all lesions were completely removed. After a mean follow-up period of 6.5 ± 3.3 (range, 4.0 to 14.8) years, the best corrected visual acuity at the final visit was 0.6 ± 0.9 logarithm of the minimum angle of resolution, and two eyes (6.3%) presented with lens opacity during follow-up.
Conclusions
In children with persistent pupillary membrane, there were no intraoperative complications, and only two patients presented with lens change during the long-term postoperative follow-up period. Surgical removal should be considered a safe and effective treatment for patients with visually significant persistent pupillary membrane.
Persistent pupillary membranes range in appearance from fine strands to densely pigmented membranes that almost fully cover the pupil, obscuring the red reflex and impairing vision [1]. Most persistent pupillary membranes require no treatment because they usually undergo atrophy during the first year of life [2]. However, some cases of persistent pupillary membranes remain visible and impair visual development; these cases require intervention such as pharmacologic therapy, laser treatments, or surgery to clear the visual axis [3,4,5,6].
In severe cases, successful surgical management with micro Vannas scissors has been reported [7]. However, this procedure carries the risks of general anesthesia, intraoperative bleeding, and intraocular infection. Furthermore, a traumatic cataract could be induced if the lens is damaged when attempting to remove the pupillary membrane [7,8,9,10,11]. To reduce the incidence of these and other surgical complications, we used vitreous scissors to remove the membrane. Vitreous scissors require a small working space in the anterior chamber and have advantages over micro Vannas scissors in preventing intraoperative complications. We are the first to report this surgical method using vitreous scissors as an alternative method to remove persistent pupillary membrane. In addition, all pupils of the operated eyes were round, and no complications such as cataract formation were found in five eyes after mean follow-up period of 22.6 months [12].
However, since this procedure involves intraocular surgery, the risk of complications persists. To date, no study has reported on the long-term surgical outcome in children with persistent pupillary membrane, including the incidence of cataract formation. Therefore, we evaluated the long-term surgical outcome and lens complications in children with persistent pupillary membrane after removal using vitreous scissors.
A retrospective medical record review was performed on children diagnosed with persistent pupillary membrane between January 1987 and December 2012 at Seoul National University Children's Hospital. Persistent pupillary membrane was defined as a thick membrane covering the pupil and arising from and inserting into the iris collarette. Patients with any other ocular anomaly such as congenital glaucoma, optic nerve disease, or congenital corneal disease that affected their visual outcome were excluded. This study was approved by the institutional review board of Seoul National University Hospital in South Korea, and the study protocol followed the tenets of the Declaration of Helsinki. The ethics committee study protocol number was 1608-146-787 and the institutional review board granted a waiver of consent for this retrospective chart review study.
At the first visit, the severity and location of the persistent pupillary membrane were evaluated and described by one experienced examiner. The visual acuity was measured using a Snellen chart, and the patients' ability to fix and follow objects was evaluated in those who were too young to apply the Snellen chart. Patients with a unilateral lesion or bilateral asymmetric lesions occluded the other eye from one hour to six hours depending on age, visual acuity, and extent of t he membrane. When t he membrane was very thick and covered the entire pupil, one drop of 2.5% mydfrin (phenylephrine hydrochloride) was administered three times a day. After at least 2 months of follow-up, the visual acuity and pupillary opening were re-evaluated. Indications for surgery included a poor visual acuity of three lines or more compared to the other eye in cases of unilateral or bilateral asymmetric lesions, a best-corrected visual acuity less than 20 / 70 in both eyes in cases with bilateral lesions, or a very thick membrane that covered the entire pupil with a pupillary opening less than 1.5 mm after mydriatics were administered. If the membrane in both eyes was so extensive that it obscured the visual axis in patients younger than 1 year, surgery was also performed.
After instillation of miotics, a 1.5-mm limbal incision was made, and viscoelastics were placed under the pupillary membrane to tent it away from the lens and above the membrane to protect the corneal endothelium. Membrane-iris adhesions were carefully dissected with the vitreous scissors and removed from the anterior chamber with microforceps [12]. All surgeries were performed by the same surgeon (YSY), and the minimum required follow-up period after surgery was 4 years.
After surgery, the visual acuity was assessed every 4 to 5 months when possible. Refraction was also evaluated at every visit, and glasses were prescribed if there were significant refractive errors, such as astigmatism or anisometropia. Patching was prescribed when a difference in visual acuity persisted while wearing glasses. Anterior segment photographs were obtained both before and after surgery when possible.
The factors we evaluated were age, sex, visual acuity, refractive errors, and complications during or after surgery. The visual acuity as measured using a Snellen chart was converted to logarithm of the minimum angle of resolution (logMAR) for analysis.
This study included 32 eyes in 26 patients. The mean age at the initial visit was 22.6 ± 34.7 (range, 0.9 to 141.2) months, and the mean age at surgery was 43.7 ± 36.0 (range, 1.0 to 142.5; median, 38.0) months. The visual acuity in 16 eyes of 10 patients was 0.5 ± 0.2 logMAR. The remaining 16 patients were too young to assess visual acuity. Cycloplegic refraction was difficult to perform in most patients because the membrane was too extensive and the reflex was very dim.
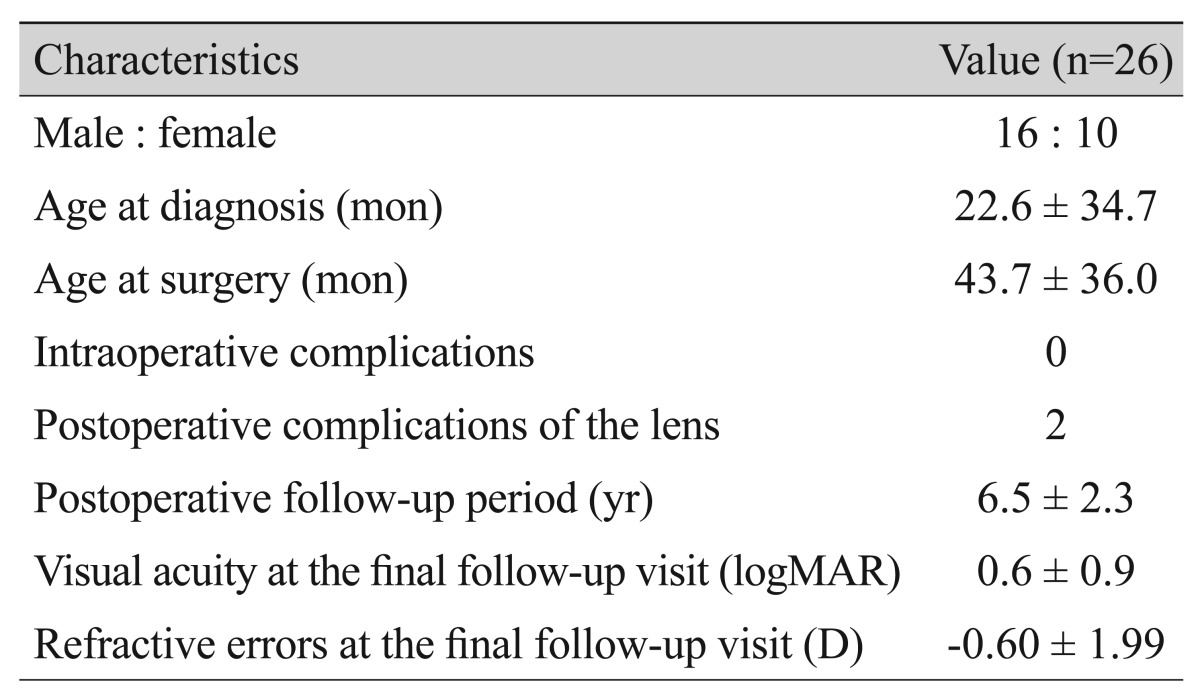
No intraoperative complications were observed using vitreous scissors, and all lesions were removed in all patients. After a mean follow-up period of 6.5 ]± 2.3 (range, 4.0 to 14.8) years, the best-corrected visual acuity at the final visit was 0.6 ]± 0.9 logMAR, and the mean refractive error was -0.60 ]± 0.99 diopters (Table 1).
At the end of surgery, the lens was clear with an intact anterior capsule in all patients. The pupils of 30 of the 32 eyes in 24 patients were round, and no complications were found after a long-term follow-up period. Only 2 eyes in 2 patients presented with lens change during follow-up.
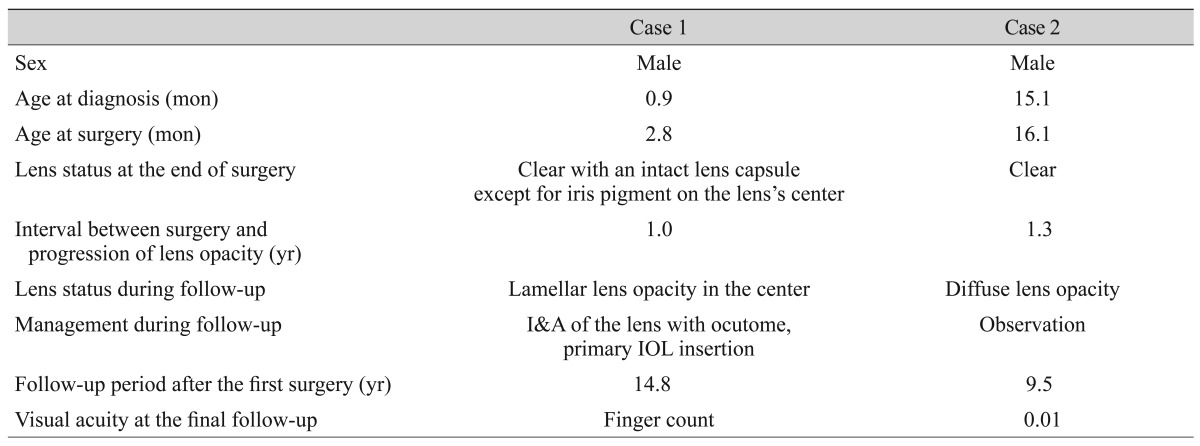
In case 1, a 1-month-old boy visited the hospital due to a persistent pupillary membrane in the right eye since just after birth. It was a unilateral lesion with a very thick membrane that covered the entire pupil, and the pupillary opening was less than 1.5 mm af ter mydr iatics were administered. At 2.8 months, he underwent removal of the persistent pupillary membrane using vitreous scissors. At the end of the procedure, the lens was clear with an intact anterior capsule, and only some iris pigments remained on the center of the lens. After 1 year, lens opacity began to appear. During 4 years of follow-up, the patient's lamellar lens opacity had progressed, leading to a decrease in visual acuity. Therefore, we performed irrigation and aspiration of the lens with an ocutome, primary intraocular lens insertion, and posterior synechiolysis. Even if we occluded the fellow eye after the second operation, the visual acuity at final follow-up (14.8 years after the first operation) was finger count in the affected eye and -0.1 logMAR in the other eye.
In case 2, a 15-month-old boy visited the hospital because of a persistent pupillary membrane in the right eye. He had a unilateral lesion covering entire the pupil, similar to case 1. Therefore, he also underwent removal of persistent pupillary membrane using vitreous scissors at 16.1 months of age. There were no intraoperative complications, and the lens was clear with an intact anterior capsule at the conclusion of surgery. After 1.3 years, lens opacity became apparent. Diffuse lens opacity progressed and produced a decrease in visual acuity. We recommended removal of the lens. However, the parents refused the operation, so we simply observed the patient for 6.5 years after the first operation. At the final follow-up, visual acuity was 2.0 logMAR in the affected eye with sensory exotropia and 0.0 logMAR in the other eye (Table 2).
The pupillary membrane forms between the lens epithelium and the corneal endothelium and replaces the vascular tunica [13]. This membrane branches from the major arterial circle of the iris. At 6 months gestation, the membrane begins to resorb, and the vessels atrophy; this process is normally complete by 8.5 months gestation. If involution is incomplete, atrophy or a remnant of the pupillary membrane can persist [13,14,15].
A persistent pupillary membrane is usually an isolated finding, and most lesions are asymptomatic. However, some persistent pupillary membranes that impair visual acuity can produce deprivation of amblyopia [6]. Management of persistent pupillary membrane depends on the extent of the membrane and therefore the size of the pupillary opening. Miller and Judisch [6] reported that mydriatics and full time occlusion therapy could obviate the need for surgery in patients with persistent pupillary membrane. They reported that mydriatic drops to maximize the pupillary opening, close monitoring of the fixation pattern, and occlusion therapy as indicated until the minimum undilated pupillary dimension is 1.5 mm should insure normal visual development. However, despite interventions like pharmacologic therapy, laser treatments, and surgery, a thick membrane that covers the entire pupil or leaves a pupillary opening less than 1.5 mm usually requires surgical removal. In the present study, we also recommended surgical removal when the pupillary opening was too small to expect normal visual development or when visual acuity was poor. Patients with good visual acuity or only a small persistent pupillary membrane did not undergo surgery.
Surgical removal carries the risk of general anesthesia, intraoperative bleeding, intraocular infection, or lens damage [7,8,9,10,11]. When numerous diffuse adhesions are present, lens damage could occur during attempts to remove the pupillary membrane. Altun et al. [16] used microscissors to severe a persistent pupillary membrane. After separation from the iris, the persistent pupillary membrane was gently peeled off the anterior lens surface using 23-gauge capsulorhexis forceps. However, the persistent pupillary membrane had adhered to the lens surface. During separation, the anterior lens capsule was damaged, and both of the patient's eyes required crystalline lens extraction during surgery. However, in the present study, there was no intraoperative complication; at the end of surgery, all lesions were completely removed, and the lens was also clear with an intact anterior capsule. The vitreous scissors used in the present study are smaller than other scissors and require only a small working space in the anterior chamber. This instrument also provides adequate force for pupillary membranectomy without damaging the lens [12].
Other previous studies have also reported that an extensive persistent pupillary membrane was surgically removed without injury to the crystalline lens and remained clear after surgery [4,9,11]. They asserted that surgical removal is effective for patients with an extensive persistent pupillary membrane. However, the postoperative follow-up period in these studies ranged from 2 to 16 months. In the present study, we observed patients for at least 4 years following the surgery. Of 32 total eyes, the lenses of 30 remained clear; only 2 eyes presented with lens opacity after 1 and 1.3 years postoperatively, respectively. Ramappa et al. [4] reported the histopathological findings in a 12-year-old boy with bilateral extensive hyperplastic persistent pupillary membrane after surgical removal without injury to the crystalline lens. They discovered that the lens capsule was unique, and the membrane adherent to the lens can have indistinguishable histologic features from portions of the lens. In our study, we assumed that microscopic damage could occur to the lens during removal in 2 patients even if the lens grossly appeared clear at the end of surgery. However, further examination including histopathologic examination would be necessary to confirm this suspicion.
Our study had several limitations. We retrospectively reviewed patients with a persistent pupillary membrane, but those with a lack of documentation were excluded. In addition, medical records that contained old anterior segment photography had been discarded due to our hospital's policy. However, other medical records, including surgical and outpatient clinic records, were fully available for analysis.
To the best of our knowledge, this is the first study to evaluate the long-term surgical outcomes and lens complications in children with persistent pupillary membrane after removal using vitreous scissors. We found no significant intraoperative complications, and only 2 patients presented with lens changes during the long-term follow-up period after removal of persistent pupillary membrane. In patients with visually significant persistent pupillary membrane, surgical removal should be considered to improve visual function.
Notes
This study was presented as an e-poster at the 116th Annual Meeting of the Korean Ophthalmological Society in 2016.
Notes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
REFERENCES
1. Viswanathan D, Padmanabhan P, Johri A. Hyperplastic persistent pupillary membranes with congenital corneal anomalies. J Cataract Refract Surg 2007;33:1123-1126.


2. Thacker NM, Brit MT, Demer JL. Extensive persistent pupillary membranes: conservative management. J AAPOS 2005;9:495-496.


3. Kraus CL, Lueder GT. Clinical characteristics and surgical approach to visually significant persistent pupillary membranes. J AAPOS 2014;18:596-599.


4. Ramappa M, Murthy SI, Chaurasia S, et al. Lens-preserving excision of congenital hyperplastic pupillary membranes with clinicopathological correlation. J AAPOS 2012;16:201-203.


5. Vega LF, Sabates R. Neodymium: YAG laser treatment of persistent pupillary membrane. Ophthalmic Surg 1987;18:452-454.


6. Miller SD, Judisch GF. Persistent pupillary membrane: successful medical management. Arch Ophthalmol 1979;97:1911-1913.


7. Reynolds JD, Hiles DA, Johnson BL, Biglan AW. Hyperplastic persistent pupillary membrane: surgical management. J Pediatr Ophthalmol Strabismus 1983;20:149-152.


8. Matsue N, Okabe S, Seki Y. Prelental fibroplasias from pupillary membrane. Jpn J Clin Ophthalmol 1973;27:37-42.
9. Oner A, Ilhan O, Dogan H. Bilateral extensive persistent pupillary membranes. J Pediatr Ophthalmol Strabismus 2007;44:57-58.


10. Kothari M, Mody K. Excision of persistent pupillary membrane using a suction cutter. J Pediatr Ophthalmol Strabismus 2009;46:187

12. Lim KH, Yu YS. Surgical management for persistent pupillary membrane with vitreous scissors. Korean J Ophthalmol 1996;10:124-126.


13. Goldberg MF. Persistent fetal vasculature (PFV): an integrated interpretation of signs and symptoms associated with persistent hyperplastic primary vitreous (PHPV). LIV Edward Jackson Memorial Lecture. Am J Ophthalmol 1997;124:587-626.


14. Robb RM. Fibrous congenital iris membranes with pupillary distortion. Trans Am Ophthalmol Soc 2001;99:45-50.


- TOOLS
-
METRICS

-
- 5 Crossref
- 0 Scopus
- 2,229 View
- 25 Download
- Related articles



 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print



