 |
 |
| Korean J Ophthalmol > Volume 30(5); 2016 > Article |
Abstract
Purpose
To describe the change of lacrimal gland volumes in Korean patients with thyroid-associated ophthalmopathy (TAO) via computed tomography (CT).
Methods
A retrospective review of CT images from 217 TAO patients and 135 control subjects was performed. The TAO patients were diagnosed between May 2005 and May 2014 and had a CT performed on initial presentation (330 orbital CT scans). These images were compared with 270 orbital CT scans from the control group, obtained between May 2013 and May 2014. An open source DICOM viewer was used to calculate the volume of the lacrimal gland.
Results
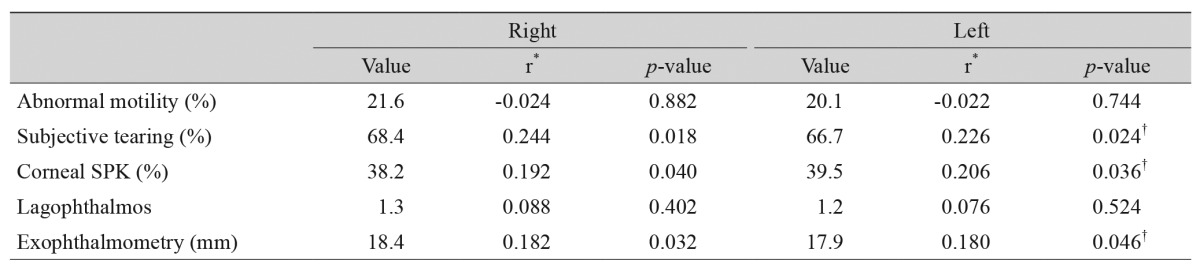
The mean volume of the lacrimal gland in TAO patients was 0.816 cm3 in the right orbit (standard deviation [SD], 0.048) and 0.811 cm3 in the left orbit (SD, 0.051), with no significant difference between right and left (p = 0.192). However, significant differences were observed between TAO patients and healthy individuals (p < 0.001). There was no significant difference between mean lacrimal gland volumes of males (0.812 cm3; SD, 0.037) and females (0.816 cm3; SD, 0.029) (p = 0.513). There was a negative correlation between gland volume and age in TAO patients (Pearson r = -0.479, p = 0.00). The subjective tearing (right: r = 0.244, p = 0.018; left: r = 0.226, p = 0.024), corneal superficial punctate keratopathy (right: r = 0.192, p = 0.040; left: r = 0.206, p = 0.036), and exophthalmometry (right: r = 0.182, p = 0.032; left: r = 0.180, p = 0.046) correlated with lacrimal gland volume.
Conclusions
This study is the first to use CT images to calculate the lacrimal gland volume of Korean TAO patients. In TAO patients, the lacrimal gland volume was notably increased compared to control subjects. The lacrimal gland volume decreased with age, but there was no difference between gender and no difference between left and right. The lacrimal gland volume correlated with subjective tearing, corneal superficial punctate keratopathy and exophthalmometry.
Thyroid-associated ophthalmopathy (TAO) is an autoimmune disease in which the thyroid stimulating hormone receptor stimulating antibody and thyroid stimulating hormone receptors influence several different cells within the orbit [1].
The disease induces an inflammatory response in the orbital tissues [2]. The lacrimal gland consists of a main gland and an accessory gland. The main lacrimal gland is further divided by the lateral horn of levator aponeurotic muscle into the orbital lobe and palpebral lobe. In addition to tear secretion, the main lacrimal gland also contributes significantly to the immune system of the ocular surface [3].
Dry eye syndrome is defined by an abnormal tear film that results in changes to the ocular surface, which can lead to ocular discomfort [4]. TAO is associated with dry eye syndrome because the proteomics of tear fluid in these patients demonstrate an upregulation of inflammatory proteins and a downregulation of protective proteins. Additionally, these patients have mechanical impairment of orbital muscles and immune-mediated lacrimal gland dysfunction. All of these factors contribute to ocular surface damage, most likely due to ocular surface inflammation [5,6,7,8]. TAO also causes an increase in gland size [9]. According to previous studies of An et al. [10], the lacrimal gland size decreases with age. The lacrimal gland size of healthy Korean individuals has been reported using brain computed tomography (CT) angiography [10] and three-dimensional orbital CT scans [11].
However, there are not many studies that focus on the lacrimal gland volumes of TAO patients using CT. Furthermore, there are no studies which focus specifically on Korean TAO patients.
Therefore, this study used CT scans to measure the volumes of lacrimal glands of Korean TAO patients and to determine the changes of volume associated with age and clinical symptoms.
This study retrospectively reviewed medical records of Korean TAO patients who had initial CT scans performed between May 2005 and May 2014. All scans were obtained from patients on initial presentation. These patients had no previous history of eyelid or orbital surgery. The control group orbital CT scans were performed between May 2013 and May 2014. As described by Bingham et al. [12], CT scans were obtained using a 2-mm slice thickness orbit protocol on a Toshiba Aquilion 64-slice scanner (Toshiba Medical Systems, Otawara, Japan). As described by Bingham et al. [13], an open source DICOM viewer (OsiriX, Geneva, Switzerland) was used to outline the lacrimal gland in consecutive axial slices and calculate the volume (Fig. 1). According to this protocol, the gland was treated as one structure because the palpebral and orbital lobes were difficult to distinguish on CT. The orbital CT scans were magnified 300% to clarify the lacrimal gland borders and thus increased the accuracy. All data were determined by averaging the values measured by two ophthalmologists (SWS and HDH). Inter-examiner reproducibility was confirmed via the intraclass correlation coefficient (ICC) using ANOVA. ICC is a value that explains the conformity of the repeated measurement values. Previously reported criteria for ICC are as follows: ICC values less than 0.4 are considered a low degree of conformity, values greater than 0.4 are considered excellent conformity and values less than 0.75 are considered perfect conformity [10,14].
Lacrimal gland volume was measured in both orbits of all subjects. The mean and standard deviation (SD) were calculated for the volume of lacrimal glands in both the right and left orbits. The distribution of lacrimal gland volume values in right and left orbits was also characterized. Clinical notes that correlated most closely to the time of the CT scan were reviewed. Data were collected for abnormal motility, subjective tearing, corneal superficial punctate keratopathy (SPK), lagophthalmos and exophthalmometry [12]. The exclusion criteria for the TAO patients included non-Korean, age <20 years, previous orbital surgery, contralateral eye of a unilateral TAO patient (i.e., no symptoms to suspect TAO on one side and no extraocular muscle hypertrophy in CT scans). The exclusion criteria for the control group included non-Korean, age <20 years, previous orbital surgery, orbital trauma history and patients with underlying medical problems that affect the volume of the lacrimal gland. For the gland volume comparison between left, right, and different sexes, the two-sample t-test was used, and the relationship between gland volume and increased age, gland volume and clinical symptoms were both analyzed by Pearson correlation coefficients (r). A p-value less than 0.05 was considered to be statistically significant.
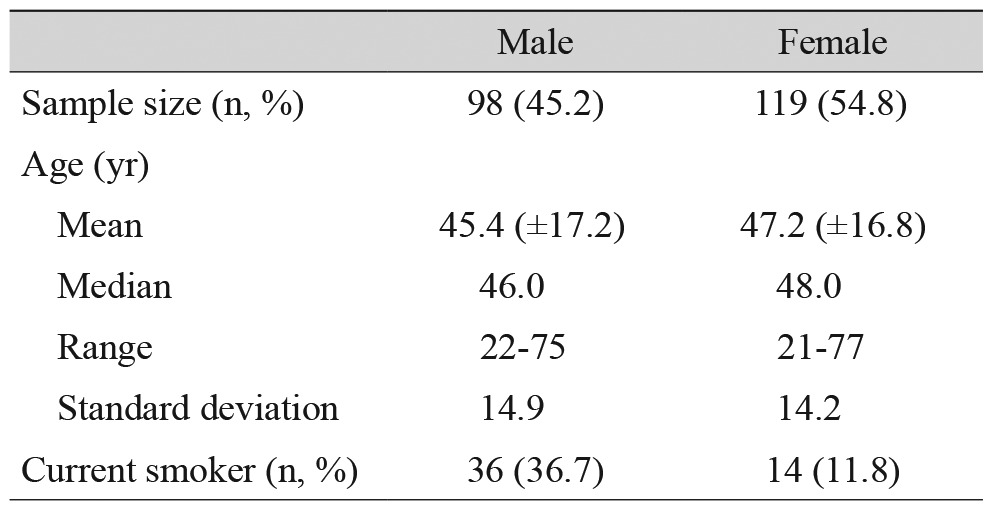
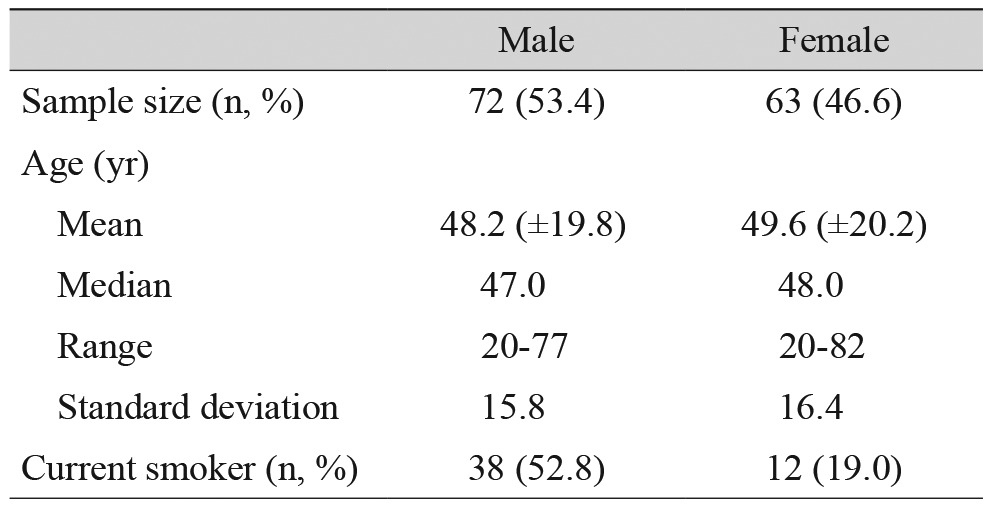
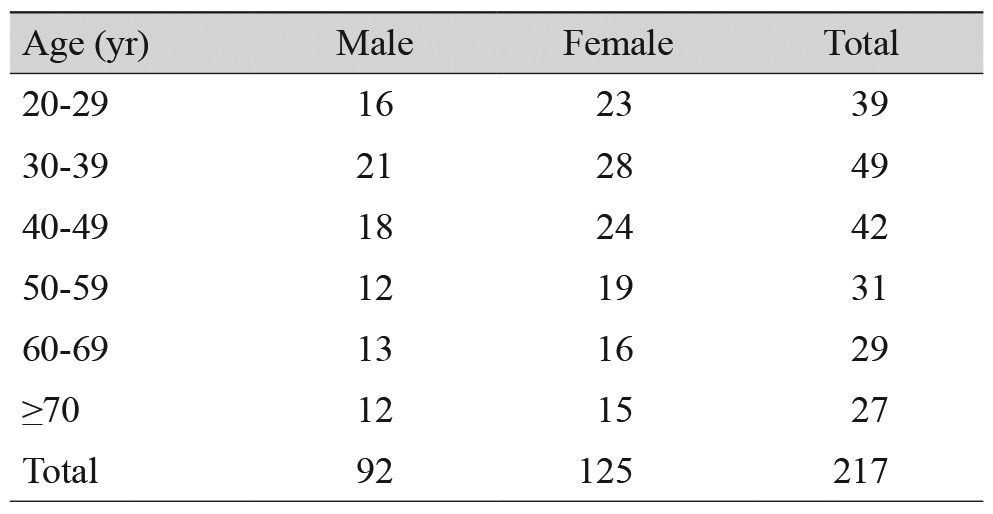
A total of 224 TAO patients were considered. Among the patients, three were less than 20 years of age, two were non-Korean, and two had a previous history of orbital surgery. After excluding these patients, 217 patients remained (434 orbits). One hundred and four normal orbits from patients with unilateral TAO were also excluded, leaving 330 orbits for analysis. The mean age was 47 ± 16.28 years (range, 21 to 77 years) and 54.8% (119 / 217) of the patients were female. Smokers represented 23% (50 / 217) of the patients. Table 1 summarizes these findings.
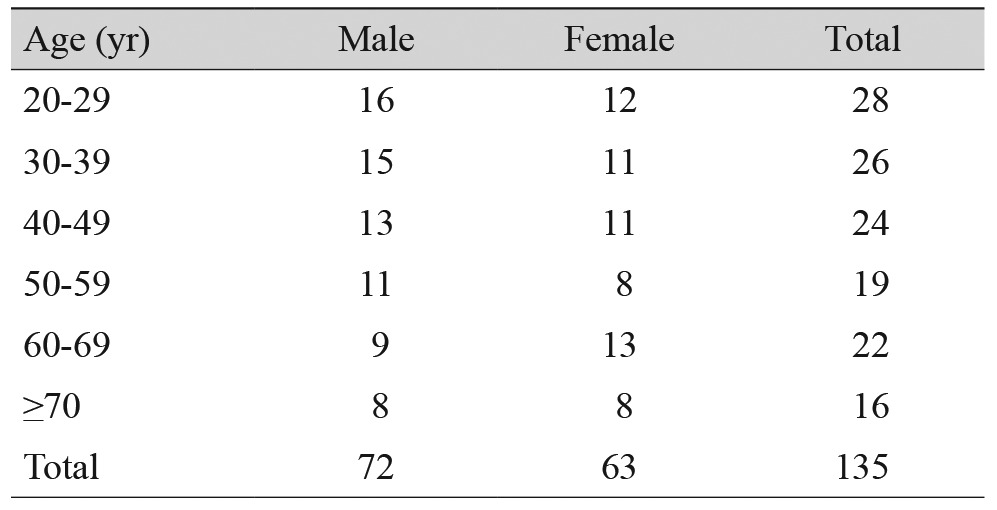
A retrospective review of a total of 725 individuals (that took orbital CT scans at clinic from May 2013 through May 2014), were less than 20 years of age, non-Koreans, had a previous history of orbital surgery history or orbital trauma history, or patients with underlying medical problems that affect the volume of the lacrimal gland were excluded; the remaining 135 normal Koreans (270 orbits) were analyzed. The mean age was 48 ± 19.98 years (range, 20 to 82 years) and 46.6% (63 / 135) of the patients were female. Smokers represented 37% (50 / 135) of the patients. These findings are summarized in Table 2. There was no significant difference between the mean age of the Korean TAO patients and the control subjects (p = 0.668).
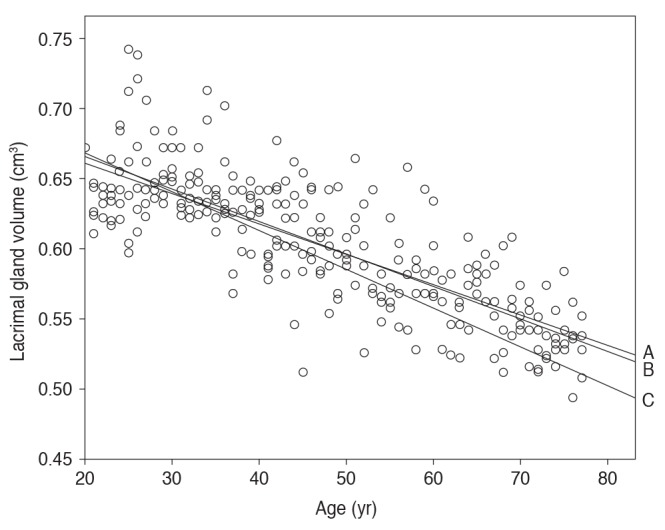
TAO Patients were classified into age groups, 39 patients in their 20s, 49 in their 30s, 42 in their 40s, 31 in their 50s, 29 in their 60s, and 27 patients were over 70 years old. Tables 3 and 4 summarize the age distribution among the TAO patients and the control subjects, respectively. The mean volume of the lacrimal gland in patients with TAO was 0.814 cm3 (SD, 0.032). The mean volume of the lacrimal gland in patients with TAO was 0.816 cm3 in right orbits (SD, 0.048) and 0.811 cm3 in left orbits (SD, 0.051), with no significant difference between right and left (p = 0.192). The mean volume of the lacrimal gland in normal Korean populations was 0.602 cm3 (SD, 0.038). The mean volume of the lacrimal gland in the control group was 0.608 cm3 in the right orbit (SD, 0.036), 0.597 cm3 in the left orbit (SD, 0.042), with no significant difference between right and left (p = 0.112). The lacrimal gland volume in patients with TAO was significantly greater compared with the control group using a two-sample t-test (p < 0.001) (Table 5). The mean volume was 0.812 cm3 in male orbits (SD, 0.037) and 0.816 cm3 in female orbits (SD, 0.029), with no significant difference in gender (p = 0.513) among TAO patients. The mean lacrimal gland volume classified by age groups in patients with TAO was 0.838 cm3 for ages 21 to 30 (SD, 0.027), 0.825 cm3 for ages 31 to 40 (SD, 0.023), 0.810 cm3 for ages 41 to 50 (SD, 0.026), 0.808 cm3 for ages 51 to 60 (SD, 0.036), 0.802 cm3 for ages 61 to 70 (SD, 0.030), 0.789 cm3 for over 70 years of age (SD, 0.028), and showed a decrease in volume with increasing age (Pearson r = -0.479) (Fig. 2). Among TAO patients, the gland volume measured in current smokers and non-current smokers was 0.827 (SD, 0.072) and 0.809 (SD, 0.032), respectively, and showed a significant difference (p = 0.02). The mean volume was 0.600 cm3 in male orbits (SD, 0.032) and 0.605 cm3 in female orbits (SD, 0.036), with no significant difference between men and women (p = 0.122) in the control group. The mean lacrimal gland volume classified by age groups in normal Korean populations was 0.649 cm3 for ages 21 to 30 (SD, 0.086), 0.637 cm3 for ages 31 to 40 (SD, 0.062), 0.606 cm3 for ages 41 to 50 (SD, 0.048), 0.587 cm3 for ages 51 to 60 (SD, 0.042), 0.561 cm3 for ages 61 to 70 (SD, 0.038), 0.536 cm3 for over 70 years of age (SD, 0.032), and showed a decreased in volume with increasing age (Pearson r = -0.802). It was observed that the gland volume decreased with increasing age in both males and females, and the ratio of decrease was greater in females (male Pearson r = -0.772, female Pearson r = -0.830) (Fig. 3). Among the control group, the gland volume measured in current smokers and non-current smokers was 0.598 (SD, 0.082) and 0.622 (SD, 0.026), respectively and was statistically significant (p = 0.01).
In the right orbit, the lacrimal gland volume correlated with subjective tearing (r = 0.244, p = 0.018), corneal SPK (r = 0.192, p = 0.040) and exophthalmometry (r = 0.182, p = 0.032). It did not correlate with abnormal motility or lagophthalmos. In the analysis of the left orbit, the lacrimal gland volume correlated with subjective tearing (r = 0.226, p = 0.024), corneal SPK (r = 0.206, p = 0.036), and exophthalmometry (r = 0.180, p = 0.046). It did not correlate with abnormal motility or lagophthalmos (Table 6).
Lacrimal gland hypertrophy can be observed in idiopathic orbital inflammation, Sjögren's syndrome, Wegener's granulomatosis, TAO, malignant and benign tumors as well as several other diseases [12,15].
Many different methods have been used to measure lacrimal gland volumes such as CT, magnetic resonance imaging, ultrasonography [13,16,17,18,19]. Tamboli et al. [16] used CT to measure normal lacrimal glands two-dimensionally and Bingham et al. [13] measured normal lacrimal glands three-dimensionally. Ueno et al. [18] reported about lacrimal gland volume and density variation by age using magnetic resonance imaging and Avetisov et al. [19] used ultrasonography to measure normal lacrimal gland volumes.
However, there is a lack of research on the relationship between lacrimal gland volumes and age in Korean TAO patients. CT is used most frequently when clinically assessing lacrimal gland and orbital diseases. Also, using CT, the actual lacrimal gland can easily be obtained within the doctor's office. Thus, the authors used CT to measure lacrimal gland volumes because of its increased utility compared to other methods. Prager suggested that the gland weight decreased with age, and Bingham et al. [13] suggested that the gland volume decreased with age [20]. Obata et al. [21] performed histopathological cadaveric research of male and female subjects, and identified extensive orbital atrophy and tissue fibrosis around the lacrimal gland which increases with age.
For these reasons, we can say that lacrimal gland volume decreases with age. Ueno et al. [18] studied males and females separately and reported that gland volume and density enhancement decreased with age in females, and suggested that this was due to hormonal changes associated with aging.
In this study, lacrimal gland volume decreased with increasing age in TAO patients. These results are similar to the results of previous studies. This negative correlation of volume change and age was observed in both male and females. However, the female group has more negative correlation than the male group. This corresponds with the suggestion by Ueno et al. [18] that hormones play a role in the development and aging of lacrimal glands. In order to discover a more accurate relationship between hormones and lacrimal gland volumes, research on gland volume and hormone levels in females before and after puberty and menopause is needed. Research on Caucasians done by Bingham et al. [13] showed that the left and right lacrimal gland volumes were 0.649 cm3 (SD, 0.231), 0.696 cm3 (SD, 0.261), respectively, and had no statistical significance. In the current study at our facility, the right gland volume was 0.816 cm3 (SD, 0.048), and left gland volume was 0.811 cm3 (SD, 0.051), and also had no statistical significance (p = 0.192). These results are similar to that of Bingham et al. [13] and we can verify that there is no difference in gland volume between left and right in TAO individuals. Dry eye is a very common symptom in TAO. Etiologies include corneal exposure from eyelid retraction and proptosis, decreased tear secretion, decreased tear break-up time, and reduced goblet cell concentration [5,6,7,8,22,23]. Thyroid stimulating hormone receptors have been reported on the surface of lacrimal gland acinar cells, and there is a strong correlation between lacrimal gland dysfunction and the presence of thyroid antibodies [23,24]. This study also demonstrated a correlation between enlargement of the lacrimal gland and the presence of corneal SPK as well as an increase in subjective tearing. The increase in subjective tearing that correlates with increased lacrimal gland volume may be reflexive tearing secondary to dry eyes. Current smoking status correlated with lacrimal gland volume, with smokers' lacrimal glands being larger. This corresponds with the findings of Planck et al. [25] and Wiersinga [26].
Smoking status is associated with TAO because immediate early genes, interleukin-1 beta, interleukin-6 are overexpressed in smokers with severe active TAO compared with nonsmokers, suggesting that smoking activates pathways associated with adipogenesis and inflammation [25,26].
This study is limited due to its retrospective nature. The lacrimal glands and surrounding tissue often demonstrate very similar densities on CT scans and makes it difficult to differentiate one another. Additionally, the specific pack year smoking history was not recorded from patients who smoked. Thus, no conclusions could be drawn regarding the amount of smoking and lacrimal gland volume. Even though this was not a large study, significant increase in lacrimal gland volume in TAO patients and decreased volume was associated with increased age in TAO patients.
In conclusion, this study presents a unique perspective, focusing on lacrimal gland volumes in Korean TAO patients measured via CT. Lacrimal gland volumes in Korean TAO patients were increased significantly compared with the control group, and decreased lacrimal gland volume was seen with increased age. The lacrimal gland volume correlated with subjective tearing, corneal SPK and exophthalmometry.
Notes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
REFERENCES
1. Bahn RS, Dutton CM, Natt N, et al. Thyrotropin receptor expression in Graves' orbital adipose/connective tissues: potential autoantigen in Graves' ophthalmopathy. J Clin Endocrinol Metab 1998;83:998-1002.


2. Bothun ED, Scheurer RA, Harrison AR, Lee MS. Update on thyroid eye disease and management. Clin Ophthalmol 2009;3:543-551.


3. Chandler JW, Gillette TE. Immunologic defense mechanisms of the ocular surface. Ophthalmology 1983;90:585-591.


4. Schaumberg DA, Nichols JJ, Papas EB, et al. The international workshop on meibomian gland dysfunction: report of the subcommittee on the epidemiology of, and associated risk factors for, MGD. Invest Ophthalmol Vis Sci 2011;52:1994-2005.



5. Matheis N, Grus FH, Breitenfeld M, et al. Proteomics differentiate between thyroid-associated orbitopathy and dry eye syndrome. Invest Ophthalmol Vis Sci 2015;56:2649-2656.


6. Selter JH, Gire AI, Sikder S. The relationship between Graves' ophthalmopathy and dry eye syndrome. Clin Ophthalmol 2014;9:57-62.


7. Ismailova DS, Fedorov AA, Grusha YO. Ocular surface changes in thyroid eye disease. Orbit 2013;32:87-90.


8. Gurdal C, Sarac O, Genc I, et al. Ocular surface and dry eye in Graves' disease. Curr Eye Res 2011;36:8-13.


9. Gupta A, Sadeghi PB, Akpek EK. Occult thyroid eye disease in patients presenting with dry eye symptoms. Am J Ophthalmol 2009;147:919-923.


10. An SH, Jin SW, Yang WS, Ahn HB. Calculated brain CT angiography volumes of lacrimal glands in normal Korean orbits. J Korean Ophthalmol Soc 2014;55:1413-1417.

11. Min SG, Ha MS. Calculated CT volumes of lacrimal glands in normal Korean orbits. J Korean Ophthalmol Soc 2015;56:1-5.

12. Bingham CM, Harris MA, Realini T, et al. Calculated computed tomography volumes of lacrimal glands and comparison to clinical findings in patients with thyroid eye disease. Ophthal Plast Reconstr Surg 2014;30:116-118.


13. Bingham CM, Castro A, Realini T, et al. Calculated CT volumes of lacrimal glands in normal Caucasian orbits. Ophthal Plast Reconstr Surg 2013;29:157-159.


14. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977;33:159-174.


15. Kim JH, Lee TS. A study of factors related to the course of graves' ophthalmopathy. J Korean Ophthalmol Soc 2011;52:255-260.

16. Tamboli DA, Harris MA, Hogg JP, et al. Computed tomography dimensions of the lacrimal gland in normal Caucasian orbits. Ophthal Plast Reconstr Surg 2011;27:453-456.


17. Harris MA, Realini T, Hogg JP, Sivak-Callcott JA. CT dimensions of the lacrimal gland in Graves orbitopathy. Ophthal Plast Reconstr Surg 2012;28:69-72.


18. Ueno H, Ariji E, Izumi M, et al. MR imaging of the lacrimal gland: age-related and gender-dependent changes in size and structure. Acta Radiol 1996;37:714-719.


19. Avetisov SE, Kharlap SI, Markosian AG, et al. Ultrasound spatial clinical analysis of the orbital part of the lacrimal gland in health. Vestn Oftalmol 2006;122:14-16.
20. Prager A. Macroscopic and microscopic investigations on senile atrophy of the lacrimal gland (preliminary report). Bibl Ophthalmol 1966;69:146-158.

21. Obata H, Yamamoto S, Horiuchi H, Machinami R. Histopathologic study of human lacrimal gland: statistical analysis with special reference to aging. Ophthalmology 1995;102:678-686.


22. Gilbard JP, Farris RL. Ocular surface drying and tear film osmolarity in thyroid eye disease. Acta Ophthalmol (Copenh) 1983;61:108-116.


23. Eckstein AK, Finkenrath A, Heiligenhaus A, et al. Dry eye syndrome in thyroid-associated ophthalmopathy: lacrimal expression of TSH receptor suggests involvement of TSHR-specific autoantibodies. Acta Ophthalmol Scand 2004;82(3 Pt 1):291-297.


24. Crowe JP, Christensen E, Butler J, et al. Primary biliary cirrhosis: the prevalence of hypothyroidism and its relationship to thyroid autoantibodies and sicca syndrome. Gastroenterology 1980;78:1437-1441.


Fig. 1
Axial computed tomography scan viewed on the DICOM viewer (OsiriX, Geneva, Switzerland) with the entire lacrimal gland outlined.
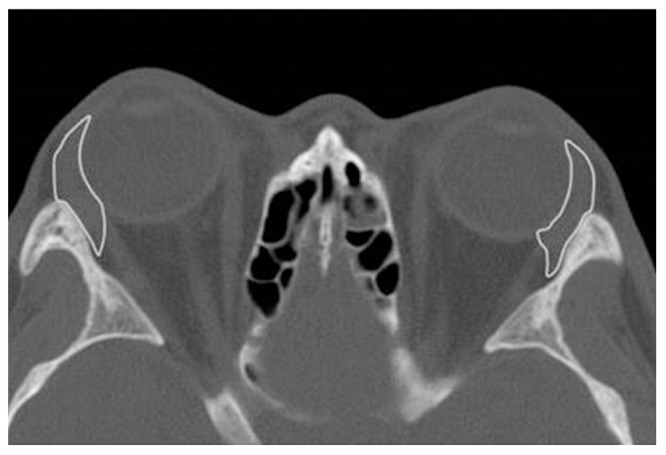
Fig. 2
Scatter plot and correlation between age and average lacrimal gland volume (cm3) in thyroid-associated ophthalmopathy (TAO) patients. B means an inverse relationship between gland volume and age in TAO patients; Pearson r = -0.479 (p = 0.00). A means an inverse relationship between gland volume and age in male TAO patients; Pearson r = -0.328 (p = 0.00). C means an inverse relationship between gland volume and age in female TAO patients; Pearson r = -0.588 (p = 0.00).
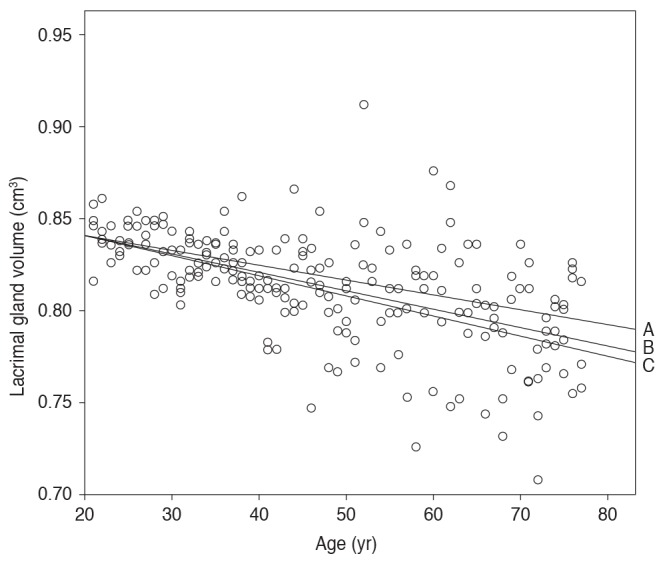
Fig. 3
Scatter plot and correlation between age and average lacrimal gland volume (cm3) in control subjects. B means an inverse relationship between gland volume and age in control subjects; Pearson r = -0.802 (p = 0.00). A means an inverse relationship between gland volume and age in male control subjects; Pearson r = -0.772 (p = 0.00). C means an inverse relationship between gland volume and age in female control subjects; Pearson r = -0.830 (p = 0.00).
- TOOLS
-
METRICS

- Related articles
-
Clinical and Genetic Findings in Korean Patients with Choroideremia2023 August;37(4)
Blood Count-derived Immunoinflammatory Markers in Thyroidassociated Ophthalmopathy2021 June;35(3)
Serum Cystatin C Concentrations in Patients with Graves’ Ophthalmopathy2020 October;34(5)
Graded Decompression of Orbital Fat and Wall in Patients with Graves' Orbitopathy2014 February;28(1)




 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print



