 |
 |
| Korean J Ophthalmol > Volume 28(6); 2014 > Article |
Dear Editor,
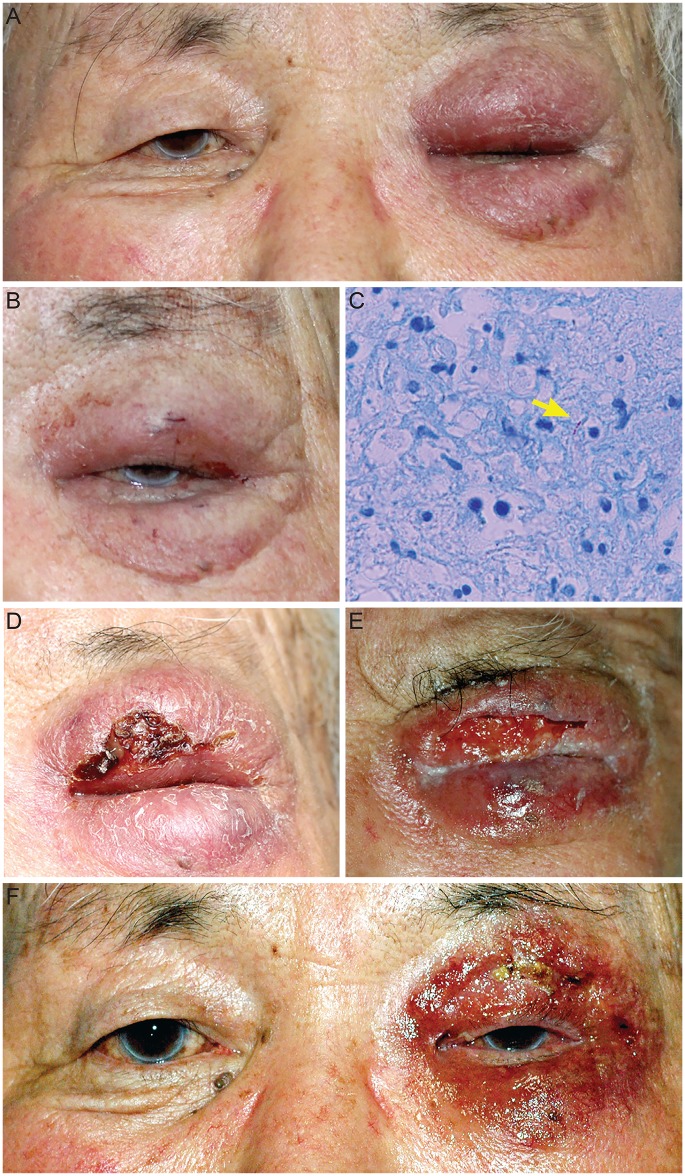
We hereby present a case of paradoxical reaction after treatment of eyelid tuberculosis (TB) with anti-TB medication. An 89-year-old man presented with painful eyelid swelling and erythema of his left eyelid, which initially developed one month earlier (Fig. 1A); he was otherwise in a healthy condition. No history of ocular trauma or operation was reported. At the time of his first visit, his corrected vision was 20 / 20 (Snellen visual acuity) in the right and 20 / 40 in the left eye. Low vision of the left eye was presumed to be attributed to a progressed cataract. Under slit-lamp examination, there were no definite abnormal ocular signs. He had moving pain, but no restriction of motion. On inspection, inflamed palpable mass was noted on the left upper and lower eyelid; however, he had no definite tenderness of the lesion. The laboratory data showed normal values (e.g., body temperature of 37℃) except a slightly elevated erythrocyte sedimentation rate of 25 mm/hr. For 3 days prior to referral to our hospital, his symptom had not been improved by intravenous administration of ceftriaxone 2 g/day. Orbit computed tomography scan with contrast showed no sign of abscess despite diffuse infiltration of upper and lower eyelids. We did a biopsy of the upper eyelid, where formation of granulation tissues was found. Pathology showed chronic nonspecific inflammation with granulomatous lesion without definite acid-fast bacilli. Under the diagnosis of anterior orbital inflammation, high dose steroid pulse therapy using 500 mg of methylprednisolone/day for 4 days was performed and the steroid dosage was tapered with oral prednisolone. Eyelid swelling and erythema improved by one month of steroidal treatment (Fig. 1B), however after discontinuation, symptoms recurred and became even worse. Biopsy was performed again under the suspicious of TB infection, and anti-TB medication, HERZ (isoniazid 300 mg, ethambutol 800 mg, rifampin 500 mg, and pyrazinamide 25 mg daily) was started immediately. The pathology result was caseous necrosis with few acid-fast bacilli (Fig. 1C), and the interferon gamma test showed was positive for the TB antigen 6.19 IU/mL. Anti-TB medication was administered for 3 weeks, however, the patient revisited the clinic complaining of serious pain and presenting skin necrosis with discharge (Fig. 1D). The patient was admitted for daily aseptic dressing of the wound and monitoring while on HERZ medication. Eyelid swelling improved slightly but wound dehiscence and oozing was aggravated 5 weeks after the initiation of HERZ treatment (Fig. 1E). Under the presumption of paradoxical response to anti-TB medication, 60 mg of prednisolone was begun with rapid tapering. Combined administration of steroid and anti-TB treatment for 1month improved wound dehiscence and reduced granulation (Fig. 1F). Thereafter, for the following 9 months, therapy included only anti-TB medication, resulting in complete resolution of infection and inflammation. However, fibrosis of the upper eyelid caused incomplete blinking.
Eyelid TB is very rare and only few cases have been reported [1]. A paradoxical response is defined as the exacerbation of the lesion or the development of a new lesion after initial improvement via anti-TB treatment [2]. It has been explained as resembling a Jarisch-Herxheimer reaction caused by the release of endotoxins after the death of organisms, followed by delayed hypersensitivity [3]. However, the accurate mechanism has not been fully understood yet. This case could be the first case report of paradoxical reaction in eyelid TB infection even though it has been described in a case of chorioretinitis associated with TB [4]. In most cases of TB pleurisy, paradoxical reaction was cured spontaneously without treatment [5]. However, in this case, oral prednisolone was required. In other case series, high dose oral prednisolone (1 mg/kg) was effective and tapered off over 12 weeks in a paradoxical reaction with TB lymphadenitis presented with tense swelling and pus in tissue [1]. As seen in our case, steroid therapy should be considered for extensive tissue damage due to paradoxical reaction.
Although eyelid TB is very rare, TB infection should be considered in cases of atypical cellulitis or severe granulation on eyelid. In addition, if patients respond inadequately or symptoms worsen while on anti-TB therapy, it is very important to consider a paradoxical response and start steroid treatment at an early stage to prevent permanent tissue damage. Of course, other potential causes such as inappropriate anti-TB regimen, incorrect diagnosis, drug resistance, and atypical mycobacterium need to be distinguished.
REFERENCES
1. Cheng VC, Ho PL, Lee RA, et al. Clinical spectrum of paradoxical deterioration during antituberculosis therapy in non-HIV-infected patients. Eur J Clin Microbiol Infect Dis 2002;21:803-809.


2. Onal IK, Bayraktar Y, Unal S. Paradoxical deterioration during the course of antituberculous treatment. J Natl Med Assoc 2006;98:954-955.


3. Fathilah J, Choo MM. The Jarisch-Herxheimer reaction in ocular syphilis. Med J Malaysia 2003;58:437-439.

Fig. 1
Representative photographs showing clinical course of the patient. (A) At initial visit left upper and lower eyelids were swollen with erythema. (B) After a month treatment of steroid, eyelid swelling and erythema was partially improved. (C) Arrow indicates acid-fast bacilli on the pathology. (D) After 3 weeks of anti-tuberculosis (anti-TB) medication, cluster and granulation formation of the upper eyelids with skin necrosis and oozing at the biopsied lesion was observed. (E) After 5 weeks of anti-TB medication, severe wound dehiscence was noted. (F) After 1 month of combined steroid and anti-TB treatment, wound dehiscence was healed and fibrosis of the upper eyelid soft tissues was observed.
- TOOLS
-
METRICS

- Related articles
-
A Case of Carotid Aneurysm in Familial Retinal Arterial Tortuosity2009 March;23(1)



 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print



