We frequently encounter uveitis patients, but the exact etiology cannot be elucidated in some cases. Uveitis after streptococcal infection has been reported in the literature. However, because of the paucity of the cases, post-streptococcal uveitis has not been well recognized by general ophthalmologists. Post-streptococcal syndrome is a systemic autoimmune disease that involves the heart, kidneys, skin, and eyes. Manifestations may include rheumatic fever, glomerulonephritis, and erythema nodosum [1]. Anterior non-granulomatous uveitis and, less frequently, posterior uveitis in young people were previously reported as manifestations of ocular involvement of post-streptococcal syndrome [2-5]. There have also been reported cases of retinal vasculitis and papillophlebitis [1,6]. Here, we describe the first case of post-streptococcal uveitis in Korea, which mainly presented with recurrent retinal vasculitis without significant anterior inflammation.
Case Report
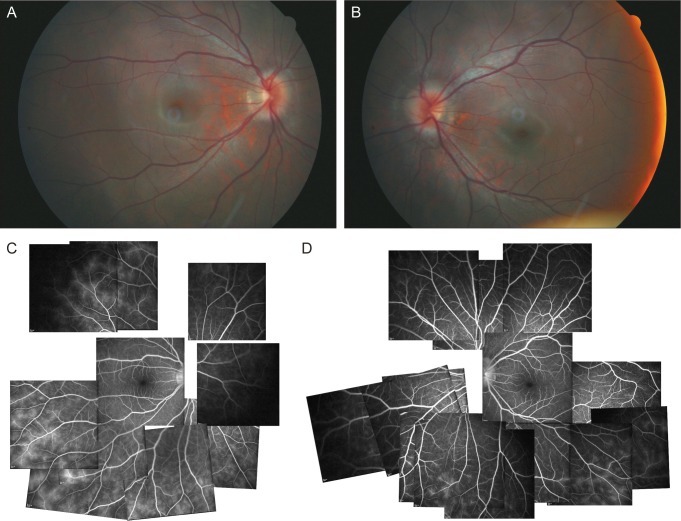
In October 2007, a 14-year-old Asian female was referred for an ophthalmological evaluation for posterior uveitis and was referred to our outpatient clinic due to decreased visual acuity. She had a history of a severe sore throat 9 months previous and subsequent proteinuria. Her initial corrected visual acuity was 20 / 30 in the right eye and 20 / 25 in the left eye. The anterior segment and lens were clear in both eyes. Cells measuring 3+ right eye and 2+ left eye were found in the vitreous. Dilated fundus exam revealed blurred disc margins with disc swelling in both eyes (Fig. 1A and 1B). Fluorescein angiography demonstrated retinal vasculitis sparing the posterior pole in both eyes (Fig. 1C and 1D). Laboratory findings showed a mild elevation of white blood cells to 6,990/mm3. Results for tuberculin skin test and serological testing for syphilis, human immunodeficiency virus, hepatitis C virus, hepatitis B virus, toxoplasmosis, cytomegalovirus, varicella zoster virus, and herpes simplex virus were all negative. The chest radiograph showed nothing significant. Elevated anti-streptolysin O (ASO) of 630 IU/mL (normal <200) and an acute phase reactant erythrocyte sedimentation rate 16 mm/hr was noted. Urinalysis and serum chemistries showed no evidence of proteinuria, and renal function was normal.
After starting steroid eye drops and oral steroid (prednisolone 1 mg/kg), her symptoms and visual acuity improved, as did the vitritis and disc swelling. Topical and oral steroids were slowly tapered. In January 2008, her corrected visual acuity improved to 20 / 20 in both eyes. Fluorescein angiography demonstrated that retinal vascular leakage was improved, and steroid treatment was stopped.
After 3 weeks, the patient visited our clinic with visual loss and infection in the right eye. In the inferior of the right eye, an anterior chamber cell score of 4+ and posterior synechiae were noted. Vitreous cells were also noted. After starting oral steroid therapy, she recovered. Her best corrected visual acuity was 20 / 20 in both eyes. Over the 1-year follow up, there was no recurrence.
Discussion
The first case of uveitis associated with post-streptococcal syndrome was described by Cokingtin and Han in 1991 [2]. In a recent case series in the literature, 28 cases of post-streptococcal uveitis were reported [4,5]. A variable spectrum of ophthalmic clinical features was noted. The largest current descriptive case series and literature review was conducted by Ur Rehman et al. [4], who identified distinguishing features of post-streptococcal uveitis as generally presenting in young patients with bilateral, non-granulomatous anterior uveitis and the presence of posterior involvement in up to one-third of cases. Post-streptococcal uveitis is thought to be associated with autoimmune disease, but the exact mechanism is not clear. Fox and associates demonstrated that chronic intraocular inflammation in rabbits could be induced by intravitreal injection of peptidoglycan-polysaccahride complexes isolated from group A streptococci [7,8].
Posterior segment involvement in large case series in the literature included focal retinitis or choroiditis [4]. Only one case of retinal vasculitis and a single case of papillophlebitis were reported both without recurrence [1,6]. The previously reported retinal vasculitis case was associated with a history of streptococcal pharyngitis and scarlet fever which had been treated with IV penicillin 2 weeks before presentation of uveitis. The case of papillophlebitis was associated with tonsillitis which had been treated with penicillin G 5 weeks prior. Our case is the first post-streptococcal uveitis reported in Korea and the third case reporting a patient presenting with inflammation mainly involving the posterior uvea.
The temporal relationship between uveitis and a previous streptococcal infection varies in the literature from 1 week to 8 weeks [4,9]. In the present case, probable streptococcal infection was reported 9 months previous, so the time lag between the streptococcal infection and uveitis was significantly longer than those in the previous reports. Patients with acute rheumatic fever and glomerulonephritis are usually treated with antibiotics to eradicate the residual streptococcal infection. Despite antibiotic treatment, the autoantibody can be triggered after a subsequent streptococcal infection. Streptococcal infection may manifest as pharyngitis, scarlet fever, or may be subclinical. In this case, the patient was sensitized after the prior streptococcal infection, and another subclinical streptococcal infection may be the causative source of the post-streptococcal uveitis syndrome.
In conclusion, post-streptococcal syndrome may be associated with posterior uveitis such as retinal vasculitis. Streptococcal infection is very common among young people, and many patients may experience subclinical infection. Recurrent posterior uveitis may cause a severe visual deficit. Therefore, in young patients, post-streptococcal uveitis should be included in the differential diagnosis of bilateral non-granulomatous uveitis or the less common posterior uveitis. A careful history should be taken, and ASO titer should be checked in members of this population with prodromal symptoms.



 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print






